Background
Some may not know that before an individual can enter chiropractic college/university, they must first attend undergraduate college. The vast majority of modern chiropractors have undergraduate degrees, primarily in the sciences (science is a requirement for chiropractic college acceptance). In fact, many chiropractic colleges/universities also have programs to educate and grant accredited undergraduate science degrees.
After undergraduate college, chiropractic college/university is an additional 4-5 year program. After completing the program and having passed all national and state board examinations, the graduate is awarded the degree of DC, which stands for Doctor of Chiropractic. Yet, while being educated, instructors often note that the DC degree actually stands for “Doctor of Chronic.” This is because chiropractors thrive on chronic pain patients, especially chronic spinal pain patients.
There is no doubt that chiropractic and spinal manipulation works well in the treating of chronic spinal pain problems, including in patients who have failed to achieve an acceptable clinical response to other more traditional approaches to their problems (1, 2, 3, 4, 5, 6, 7, 8, 9). There are a number of published plausible explanations for these outcomes, including:
- Improved motion disperses the accumulation of algogenic inflammatory chemicals that otherwise would contribute to the firing of the pain afferents (10).
- Improved motion initiates a neurological sequence of events that “closes” the pain gate (2, 3).
- Spinal adjusting (specific manipulation) activates the suprasegmental descending inhibitory control of pain (11, 12, 13).
A new plausible explanation is evolving, and this article explores it: Genetics.
••••••••••
Questions
Why do two individuals of similar physique, age, fitness, etc., injured in the same accident, have completely different post-event pain presentations?
Why do two individuals of similar physique, age, fitness, etc., after receiving similar injury (let’s say a sprained ankle or a whiplash neck injury), have very different pain recovery times? (One may recover in days to weeks, the other takes months or even years).
Are there scientific, physiological explanations that account for individual variation in pain recovery rates?
Why do so many chronic pain patients gravitate towards chiropractic? And what are some of the evolving explanations as to why chiropractic helps such individuals?
••••••••••
Biology 101
Our structure, hormones, neurotransmitters, enzymes, and more, are made up of proteins. All told, the human body uses about 22,000 proteins.
Proteins are derived from building blocks called amino acids.
The amino acids that are used to build our proteins come from our diet. (Some of these amino acids are essential, meaning that they must come from our diet; others can be manufactured in our body from other molecules, primarily other amino acids).
When humans consume protein in the diet, our digestive system breaks the protein down into its individual amino acids.
These dietary amino acids are reassembled into the approximate 22,000 proteins that the human body requires to run efficiently.
The reassembly of these amino acids into the functional proteins of life is the job of the human genome, our genetic material. Our genes are essentially a protein assembly factory.
Stated differently, approximately 22,000 human genes code for (assemble) approximately 22,000 proteins.
Our genetic material is often referred to as DNA, an abbreviation for deoxyribonucleic acid. A component of this deoxyribonucleic acid is the nucleotide bases.
Even though there are only four different nucleotide bases that make up the human genome, their total number is approximately 3 billion. Essentially, approximately 3 billion nucleotide bases code for (assembling) approximately 22,000 proteins. (Not all nucleotide bases code for protein, some is quiescent, or non-coding, or “junk [probably not]” or not yet understood).
All of this genetic material (nucleotide bases) is packed into 23 pairs of chromosomes. Each cell in our body (about 75 trillion of them) has a complete copy of all 23 chromosomes with its approximate 3-billion nucleotide bases. (There are two exceptions. Red blood cells [approximately 25 trillion of them] contain no genetic material. Sex cells have only one copy of the 23 chromosomes, not a pair; the pair is reestablished when the parents conceive a baby).
When assembling a protein, each amino acid building block is assigned to three adjacent nucleotide bases. The three nucleotide bases that are hooked up to one amino acid is call a codon. The section of a chromosome that codes (assembles) a single protein is called a gene. An example of putting it all together:
- Insulin is a protein.
- Insulin is comprised of 51 amino acids.
- The gene that codes (assembles) for insulin is 153 nucleotide bases long (51 X 3).
Damage to the nucleotide bases of the DNA alters the assembly of the proteins of life. This is the rationale for minimizing exposure to ionizing radiation, free radicals, toxic chemicals, etc.
All proteins of life are important. The emphasis of this paper is a special class of proteins called enzymes.
Enzymes are proteins that act to help the body complete metabolic/biochemical processes. Our life is not possible without these enzymes. The biochemistry of life, without enzymes, would require so much heat or so much pressure that either would kill us.
All enzymes are proteins, meaning that we have a gene that codes for (assembles) them. When reading science, one can always identify enzymes because they end in the letters ase.
All episodes of CSI or any other crime television program emphasize there are differences in each of our DNA, or specifically in the nucleotide base sequence of our DNA. These differences account for the differences between people, such as height, eye-skin-hair color, etc. The point of this discussion is that in a similar fashion, each of us has a different expression (assembling) of the genes that code for (assembles) enzymes. One such enzyme has become particularly important in the understanding of the benefits of the chiropractic adjustment in the treatment of chronic pain.
••••••••••
Physiology
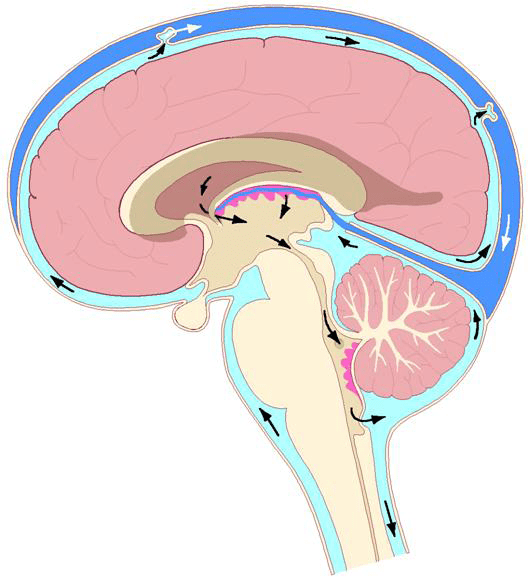
Pain is an electrical signal in the brain. Oversimplified, five structures are involved for the pain electrical signal to reach the brain:
The Receptor
The receptor converts an environmental stress into the electrical signal.
- For chronic low back pain the receptor is primarily in the intervertebral disc.
- For chronic neck pain the receptor is primarily in the facet.
- Receptor thresholds are usually linked to inflammation.
The Primary Afferent Neuron
The primary afferent neuron brings the electrical signal from the receptor to the spinal cord.
- The threshold of the primary afferent neuron is influenced genetically. [Key Concept For This Paper]
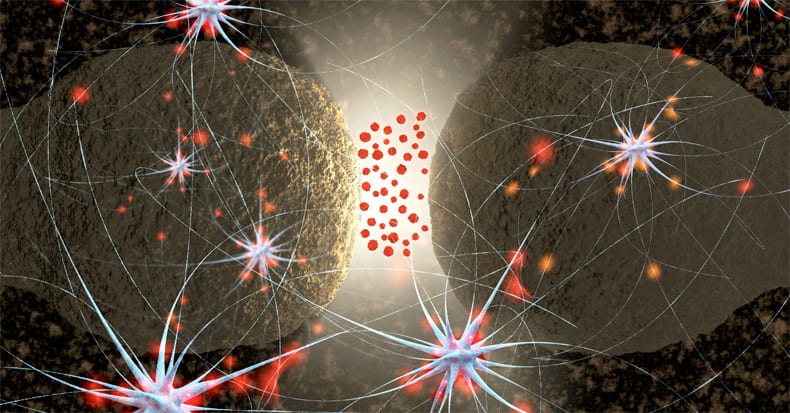
The Synapse
The synapse is the gap between the primary afferent neuron and the second order afferent neuron.
The Second Order Afferent Neuron
The second order afferent neuron brings the electrical signal from the synapse to the brain for the perception of pain.
The Brain for the perception of pain
The brain perceives the electrical signal of pain.
- Several brain relays are involved and influence both pain location and suffering.

Important for this discussion, the threshold and sensitivity of the primary afferent neuron is influenced by a chemical called norepinephrine (noradrenaline). Norepinephrine is produced by post-ganglionic sympathetic neurons. Norepinephrine makes the primary afferent neuron more sensitive, or making more painful, increasing the pain electrical signal to the brain:

••••••••••
Genetics
Increasingly, individual differences in the intensity, duration and recovery from pain syndromes is being attributed to genetic differences, and specifically to the production of particular enzymes that influence the electrical threshold and transmission of the pain neurons. The genetics of pain is detailed in the 5th edition of the book Wall and Melzack’s Textbook of Pain, 2006 (14). Chapter 9 is titled “The Genetics of Pain.” The summary of this book includes:
“Pain is associated with considerable variability between individuals. Humans exhibit robust differences in their thresholds and tolerances to controlled noxious stimuli, in their analgesic response to drugs, and in their susceptibility to (and severity of) clinical pain syndromes.”
Pain genetics is better understood in the 2014 book by Judy Foreman, titled “A Nation in Pain.” Her pertinent chapter, chapter 3 is also titled “The Genetics of Pain.” (15) Ms. Foreman notes that genetics influence both the susceptibility and sensitivity to pain, which she defines as:
Genetic susceptibility means the likelihood that you’ll get a chronic pain condition.
Genetic sensitivity means how much it hurts if you do have a chronic pain condition.
On this topic, Ms. Foreman states:
“Scientists now think that genes control perhaps 50 percent of susceptibility to chronic pain.”
“Across a number of different kinds of pain, genes seem to be at least half the driver of how much pain you experience.”
In her review of the literature, Ms. Foreman notes that a “favorite gene of pain geneticists is COMT.”
COMT is an enzyme. It’s the abbreviation for:
Catechol-Oxygen-Methyltransferase = Catechol-O-Methyltransferase
In review, note that this enzyme ends in the suffix ase, further establishing that it is a protein, and as such there is a gene that codes for (assembles) it. And all genes express differently person to person. Apparently the individual expression of COMT can significantly alter one’s sensitivity to pain. Ms. Foreman states:
“We all have the COMT gene, but some people have a form of the gene with high activity, and some, the form with low activity.”
“High activity is better! High COMT means low pain and low COMT means high pain.”
“The luckiest 40 percent of Caucasians have the high-activity form and are relatively unsusceptible to pain.” These individuals are only half as likely as others to develop chronic pain syndromes.
COMT works in part by making enzymes that get rid of stress hormones like norepinephrine. “Since norepinephrine acts directly on nervesóthus boosting painógetting rid of norepinephrine can reduce pain.”
“There’s another key finding emerging from the COMT research. The hormone estrogen decreases COMT activity. Because lower COMT means more pain, this may partly explain why women, who have more estrogen, experience more pain than men.”
In review, pain sensitivity is controlled genetically by the production of enzymes, and one such enzyme is COMT. Chronic pain is linked to the neurotransmitter norepinephrine, which is produced by the post-ganglionic sympathetic efferent neurons. Norepinephrine makes pain afferents more sensitive. Consequently, more neurotransmitter norepinephrine means more pain; less neurotransmitter norepinephrine means reduced pain. COMT degrades norepinephrine and results in less pain.
The evidence that increased genetic production of COMT inhibits pain, and reduced genetic production of COMT increases pain, is quite strong. A search of the National Library of Medicine (April 10, 2017) using the key words “COMT and Pain” located 233 studies pertaining to the topic. A sampling of these studies includes:
COMT val158met genotype affects mu-opioid neurotransmitter responses to a pain stressor. Science, 2003
Genetic influence on variability in human acute experimental pain sensitivity associated with gender, ethnicity and psychological temperament. Pain, 2004
Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum Mol Genet, 2005
Catechol-O-methyltransferase gene polymorphisms are associated with multiple pain-evoking stimuli. Pain, 2006
Genetic variation in the catechol-O-methyltransferase (COMT) gene and morphine requirements in cancer patients with pain. Mol Pain, 2008
Variation in the COMT gene: implications for pain perception and pain treatment. Pharmacogenomics, 2009
Catechol-O-methyltransferase and pain. nt Rev Neurobiol, 2010
Effect of catechol-O-methyltransferase polymorphism on response to propranolol therapy in chronic musculoskeletal pain: a randomized, double-blind, placebo-controlled, crossover pilot study. Pharmacogenet Genomics, 2010
Catechol O-methyltransferase haplotype predicts immediate musculoskeletal neck pain and psychological symptoms after motor vehicle collision. J Pain, 2011
COMT genetic variants and pain. Drugs Today (Barc), 2011
Genetic contribution of catechol-O-methyltransferase variants in treatment outcome of low back pain: a prospective genetic association study. BMC Musculoskelet Disord, 2012
Complex multilocus effects of catechol-O-methyltransferase haplotypes predict pain and pain interference 6 weeks after motor vehicle collision. Neuromolecular Med, 2014
A novel catechol-O-methyltransferase variant associated with human disc degeneration. Int J Med Sci, 2014
Genes associated with persistent lumbar radicular pain; a systematic review. BMC Musculoskelet Disord., 2016
The inference from these studies is that chronic pain susceptibility may be determinable through genetic testing.
••••••••••
The Chiropractic Connection
Increased production and release of the neurotransmitter norepinephrine increases one’s sensitivity to pain.
COMT is an enzyme that degrades the neurotransmitter norepinephrine. Increased COMT decreases norepinephrine. Reduced norepinephrine reduces pain sensitivity.
The chiropractic connection is, that it is now conclusive that chiropractic spinal adjusting (specific manipulation) reduces the production of the pain sensitizing neurotransmitter norepinephrine. Improvements in spinal mechanical function inhibit the production of norepinephrine, which would make it easier for one’s genetic ability to produce COMT to further reduce the presence of norepinephrine.
Chiropractic spinal adjusting inhibits the production of norepinephrine.
COMT degrades the norepinephrine that is produced.
Both reduce the sensitivity of the pain afferents, reducing the perception of pain in the brain.
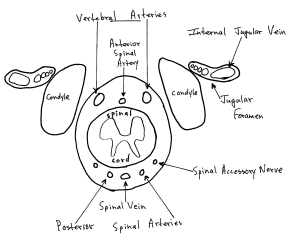
Studies showing that spinal adjusting reduces the production of norepinephrine have been in the literature for decades (16, 17, 18, 19). The most often cited explanation for this is that there exists a reflex between the articular mechanoreceptors and the sympathetic nervous system pre-ganglionic cell bodies in the gray matter of the spinal cord. This connection has been proven to exist in two-legged animals (20).
The most recent studies showing that chiropractic spinal adjusting inhibits the production of neurotransmitter norepinephrine (2011 and 2017),
use sophisticated modern technology (radioactive glucose, PET scans, and levels of salivary amylase). The authors are from the Division of Cyclotron Nuclear Medicine, Tohoku University (Graduate School of Medicine), Sendai, Japan. Their first study was published in the journal Alternative Therapies Health Medicine, and titled (21):
Cerebral Metabolic Changes in Men
After Chiropractic Spinal Manipulation for Neck Pain
The study conclusion includes:
“In summary, the present study demonstrated sympathetic relaxation [inhibition] and corresponding regional brain metabolic changes, as well as reduced muscle tone and decreased pain intensity following a chiropractic spinal manipulation.”
This group’s second study was published in the journal Evidence-Based Complementary and Alternative Medicine, and titled (22):
Glucose Metabolic Changes in the Brain and Muscles of Patients with Nonspecific Neck Pain Treated by Spinal Manipulation Therapy: A [18F]FDG PET Study
The study conclusions include:
“Brain processing after spinal manipulative therapy may lead to physiological relaxation via a decrease in sympathetic nerve activity.”
“Our assessment of body responses in this study showed relaxation of muscle tension and decreased salivary amylase levelsóphenomena that are associated with reduced sympathetic nerve activity.”
Spinal manipulative therapy stimuli to the joints may result in “decreased sympathetic nerve activity.”
The study has four important findings:
- Chiropractic adjusting inhibits muscle tone, improving ranges of motion.
- Chiropractic adjusting inhibits sympathetic tone.
- Chiropractic adjusting inhibits pain.
- The brain is affected by chiropractic adjusting.
Conclusion
The contention that chiropractic spinal adjusting reduces musculoskeletal pain is now irrefutable. The physiological mechanisms by which chiropractic adjusting helps pain patients are still being investigated and are not fully understood. It is probable that multiple mechanisms are occurring simultaneously. Inhibition of sympathetic nervous system tone with a concomitant reduction of the pain enhancing neurotransmitter norepinephrine, the topic of this paper, has both supportive evidence and biological plausibility.
REFERENCES
- Edwards BC; Low back pain and pain resulting from lumbar spine conditions: a comparison of treatment results; Australian Journal of Physiotherapy; September 1969; Vol. 15; No. 33; pp. 104-110.
- Kirkaldy-Willis WH, Managing Low Back Pain, Churchill Livingstone, 1983, p. 19.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Meade TW, Dyer S, Browne W, Townsend J, Frank OA; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; Volume 300, June 2, 1990, pp. 1431-7.
- editors; Chiropractors and Low Back Pain; Lancet; July 28, 1990; Vol. 336(8714);p. 220.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ëwhiplash’ injuries; Injury; Vol. 27; No. 9; November 1996; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999, pp. 22-25.
- Giles LGF, Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine; July 15, 2003; Vol. 28; No. 14; pp. 1490-1502.
- Muller R, Lynton G.F. Giles LGF, DC, PhD; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics, January 2005, Vol. 28, No. 1; pp. 3-11.
- Cyriax, James; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Vol. I; eighth edition; 1982.
- Vicenzino B, Collins D, Wright A; The Initial Effects of a Cervical Spine Manipulative Physiotherapy Treatment on the Pain and Dysfunction of Lateral Epicondylalgia; Pain; November 1996; Vol. 68; No. 1; pp. 69-74.
- Savva C, Giakas G, Efstathiou M; The role of the descending inhibitory pain mechanism in musculoskeletal pain following high-velocity, low amplitude thrust manipulation: a review of the literature; Journal of Back Musculoskeletal Rehabilitation; 2014; Vol. 27; No. 4; pp. 377-382.
- Garcia DV, Dierckx R, Otte a, Holstege G; PET and SPECT in Neurology, Chapter 46 “Whiplash: Real or Not Real: A Review and New Concept”; Springer-Verlag; 2014, pp. 947-963.
- Mogil JS, Mitchell B. Max MB; “The Genetics of Pain,” Chapter 9, in Wall and Melzack’s Textbook of Pain, 5th edition, edited by McMahon SB, Koltzenberg M; Elsevier Churchill Livingstone; 2006.
- Judy Foreman; A Nation in Pain; Healing Our Biggest Health Problem; Oxford University Press; 2014.
- Korr IM; Proprioceptors and somatic dysfunction; J Am Osteopath Assoc. 1975 Mar;74(7):638-50.
- Korr IM; The spinal cord as organizer of disease processes: III. Hyperactivity of sympathetic innervation as a common factor in disease; J Am Osteopath Assoc. 1979 Dec;79(4):232-7.
- Budgell B, Hirano F; Innocuous mechanical stimulation of the neck and alterations in heart-rate variability in healthy young adults; Autonomic Neuroscience; Aug 13, 2001; Vol. 9l No. 1-2; pp. 96-99.
- Koch LE, Koch H, Graumann-Brunt S, Stoll D, Ramirez JM, Saternus KS; Heart rate changes in response to mild mechanical irritation of the high cervical spinal cord region in infants; Forensic Science International; Vol. 128; No. 3; August 28, 2002; pp. 168-176.
- Jiang H, Moreau M, Raso J, Russell G, Bagnall K; Identification of the location, extent, and pathway of sensory neurologic feedback after mechanical stimulation of a lateral spinal ligament in chickens; Spine; January 1, 1997; Vol. 22; No. 1; pp. 17-25.
- Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, Itoh M, Fukuda H, Yanai K; Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain; Alternative Therapies Health Medicine; Nov-Dec 2011; Vol. 17; No. 6; pp. 12-17.
- Inami A, Ogura T, Watanuki S, Masud M, Shibuya K, Miyake M, Matsuda R, Hiraoka K, Itoh M, Fuhr AW, Yanai K, Tashiro M; Glucose Metabolic Changes in the Brain and Muscles of Patients with Nonspecific Neck Pain Treated by Spinal Manipulation Therapy: A [18F]FDG PET Study; Evidence-Based Complementary and Alternative Medicine; Volume 2017 [epub].