Chiropractic Applications
Janet Travell, MD, is one of the most recognized physicians of modern history. Her notoriety is attributed primarily to two events:
- Myofascial problems and its consequent symptoms are nearly a universal human experience. Dr. Travell was an early pioneer in understanding the science, pathophysiology, and treatment of myofascial problems. She has been referred to as “the mother of myofascial trigger point knowledge”(1).
- President John F. Kennedy suffered from a notorious bad back. His back problems significantly worsened by his legendary heroism in August of 1943 during the sinking of his boat PT-109 in the Pacific during WWII. Injured (he was awarded the Purple Heart for the event) Kennedy twice swam for miles in the Pacific Ocean, towing an injured crewmember with a life jacket strap in his teeth. Kennedy’s back problems never fully recovered. In 1954, Kennedy underwent an attempted spinal fusion operation, and it went badly; it was his second spinal surgery for his persistent low back pain. He nearly died, and his recovery took 8 months. The following year, Kennedy came under the care of myofascial pain expert Janet Travell, MD. When Kennedy was elected president of the United States (taking office in 1961), he chose Dr. Travell to be his personal White House Physician. Dr. Travell was the first female physician to hold this prestigious office (2, 3, 4).
Dr. Janet Travell was born in New York in 1901, the daughter of a physician. She died in 1997 at the age of 96. In 1926, she received her MD degree from the Cornell University Medical College in New York City, where she graduated at the head of her class. Interestingly, she was the first female to graduate from Cornell. In the first three decades of her professional career she practiced cardiology while teaching pharmacology at Cornell. Her interest in musculoskeletal pain came about as a consequence of the neck, trunk, shoulder, and arm pains her cardiac patients suffered (5).
In 1942, 1946, and 1948, Dr. Travell and colleagues reported a series of clinical outcomes following trigger point treatment in cardiac patients (6, 7, 8). Her successful outcomes led her to believe that she was treating more than somatic pain; she believed that she was also influencing aspects of the cardiac pain itself: “in patients suffering from the pain of myocardial infarction convinced her and her colleagues that the treatment could stop both non-cardiac pain of muscle origin and true cardiac pain of coronary insufficiency.”(9) This understanding is important because if true, it would mean that trigger point therapy was influencing aspects of the sympathetic nervous system.
In 2003, Dr. Travell’s colleague and co-author of their books, David Simons, MD, Myofascial pain and dysfunction, the trigger point manual, commented:
Trigger point therapy “could suppress cardiac arrhythmias. On several occasions, I saw the conversion of atrial fibrillation to normal rhythm when vapocoolant spray was applied over the arrhythmia TrP on the lower-right anterior chest wall; the same effect could be achieved by trigger point pressure release applied to that TrP. For several reasons, it appears likely that many such unexpected influences, to and from TrPs, depend on modulation of the autonomic nervous system, in addition to modulation of the sensory nervous system (referred pain).”
“The pain patterns of the pectoralis major and pectoralis minor muscles mimic the pain referral patterns of cardiac ischemia.”
“Symptoms of angina in the absence of demonstrable cardiac disease should be considered as likely due to TrPs.”
By 1952, Dr. Travell’s clinical interest and practice had moved away from cardiology and she became a specialist in musculoskeletal pain syndromes. With her growing positive reputation and expertise, Senator John F. Kennedy’s orthopedic surgeon asked Dr. Travell to look at his patient’s chronic, disabling back problems (5). Dr. Travell treated Senator Kennedy’s trigger points and addressed a number of mechanical issues that perpetuated these trigger points (discussed below).
When Dr. Travell first saw Senator Kennedy in May of 1955, he was non-ambulatory. He had suffered from 2 devastating spinal surgeries, yet he continued to suffer from debilitating back spasm and left leg pain. Things were so bad that Senator Kennedy was “questioning his ability to continue his political career.”(10) Dr. Travell treated Senator Kennedy’s trigger points. His improvement was so impressive that Dr. Travell’s daughter wrote (5):
“Senator Kennedy received so much relief of pain from my mother’s medical treatments that he had ‘new hope for a life free from crutches if not from backache’.”
In 2003, James Bagg wrote this, pertaining to Dr. Travell (10):
“Jack Kennedy saw a great many physicians over the course of his short life, but one of them, according to his brother Bobby, enabled Jack to become President of the United States.”
Kennedy considered Travell to be a medical genius (5). When Kennedy was elected to the presidency of the United States, he asked Dr. Travell to be his personal White House Physician, becoming the first woman and one of the few civilians (non military) to hold that post. After President Kennedy’s assassination in 1963, his successor, President Lyndon B. Johnson, asked Dr. Travell to stay on in the White House as his physician. A year and a half later, she resigned to return to private practice and to the position of Associate Clinical Professor of Medicine at George Washington University. She became Emeritus Clinical Professor of Medicine 1970–1988, and Honorary Clinical Professor of Medicine from 1988 until her death in 1997. Dr. Travell remained professionally active until the end of her life, writing articles, giving lectures, and attending conferences.
The enduring pinnacle of Dr. Travell’s work occurred during her years at George Washington University. She had teamed up with ex-Air Force Flight Surgeon David G. Simons, MD, to write the most authoritative text pertaining to myofascial pain syndromes and their relationship to trigger points. During their corroboration, Dr. Simons was Clinical Professor in the Department of Physical Medicine and Rehabilitation at the University of California, Irvine. This book is 713 pages in length and details anatomy, neurology, physiology, and treatment of trigger points and myofascial pain syndromes. It was published in 1983, and titled (12):
Myofascial Pain and Dysfunction:
The Trigger Point Manual
A decade later, in 1992, Volume 2 of their book (607 pages) was released, and titled (13):
Myofascial Pain and Dysfunction:
The Trigger Point Manual:
THE LOWER EXTREMITIES
In 1999, two years after Dr. Travell’s death, the final volume of the text was released (1038 pages), and titled (14):
Travell & Simons’Myofascial Pain and Dysfunction
The Trigger Point Manual:
Volume 1, Upper Half of Body
The title page of this volume includes these words:
“Dr. Janet Travell’s genius and medical insight identified in the first edition the clinical picture of individual myofascial pain syndromes and many perpetuating factors. In addition, we were most fortunate to have had the benefit of her advice in preparing some of this edition. She emphasized the importance of including a new chapter that covers the respiratory muscles and supplied unique pearls of clinical wisdom that sprinkle this revision.”
An overly simplified statement of Dr. Travell’s work is that the trigger point was able to cause muscle shortening, and that muscle shortening would as a rule cause chronic myofascial pain. People so inflicted with these trigger points and subsequent myofascial pain syndromes were chronic because conventional medical treatment did not address the root cause of the problem, the trigger point. The patient’s symptoms and signs would only resolve if the trigger point was successfully addressed.
Initially, Dr. Travell’s approach to the trigger point problem was to inject it with small amounts of procaine. Later she emphasized less invasive approaches such as the “spray and stretch” technique and “ischemic compression.”
The spray and stretch technique involved the use of “vapocoolant” while stretching the involved muscle. This cold “neurological distraction” allowed enough stretching of the interdigitation of the contractile proteins of the muscle to abort the trigger point, resulting in long-term muscle relaxation and ending the chronic pain cycle.
Ischemic compression on the trigger point (sustained pressure for a minute or two) would deprive the trigger point of the oxygen required to maintain the local contraction. The contracted fibers of the trigger point would “give up”, allowing the entire muscle to relax, again resulting in long-term muscle relaxation and ending the chronic pain cycle.
These newer trigger point ending techniques were less invasive and quickly became very popular with non-allopathic health care providers, especially chiropractors. James Bagg noted (10):
“Her [Travell’s] contributions are perhaps more widely known and appreciated by chiropractors and massage therapists than by her fellow physicians.”
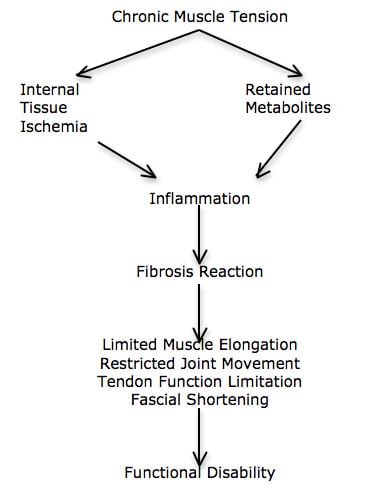
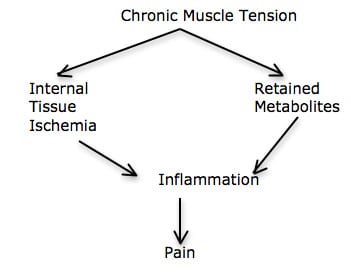
Dr. Travell notes that not only are the trigger points generators of pain, but she agrees with the writings of Rene Cailliet, MD (18); both contend that a chronically contracted muscle will cut off its own blood supply, resulting in both internal ischemia and an accumulation of metabolites. Muscle ischemia and retained metabolites create an inflammatory reaction, altering the nociceptive threshold, generating pain. Release of the trigger point and the muscle tightness reverses this process.
•••••••••
The Contributions of C. Chan Gunn, MD
- Chan Gunn, MD, is a Clinical Professor, Multidisciplinary Pain Center at the University of Washington Medical School, Seattle, WA. In his 1996 book titled (11):
The Gunn Approach to the Treatment of Chronic Pain:
Intramuscular Stimulation for Myofascial Pain of Radiculopthic Origin
In this book, Dr. Gunn added to Travell’s work on the understanding and treatment of trigger points and myofascial pain syndromes. In agreement with Travell he notes that myofascial pain syndromes cause musculoskeletal pain. He states:
“A crucial ingredient of myofascial pain is muscle shortening from contractures. In fact, myofascial pain does not exist without [muscle] shortening.”
“Chronic pain is never present without associated muscle shortening from contracture.”
“Prolonged muscle shortening can not only cause pain in muscle, it also mechanically pulls on tendons, thereby straining them and distressing the joints they act on. The increased wear and tear in joints eventually leads to degenerative changes (e.g. osteoarthritis).”
Muscle shortening can cause a large variety of pain syndromes by its relentless pull on various structures.
Muscle shortening is the key to myofascial pain. “Stated differently, pain cannot exist in the absence of muscle shortening—no shortening, no pain.”
“Muscle shortening is a fundamental feature of musculoskeletal pain.”
“Muscle shortening is an inherent component of persistent musculoskeletal pain, and its release is central to treatment.”
“An important source of pain in musculoskeletal pain syndromes is from muscle shortening that mechanically stresses muscle attachments, causing conditions such as bicipital tendonitis and lateral epicondylitis.”
“Shortening in muscles acting across a joint can upset alignment, and can precipitate pain in the joint, i.e. arthralgia.”
“Muscle shortening can eventually bring about joint degeneration—osteoarthritis.”
“Shortening of paraspinal muscles acting across a disc space compresses the disc and can cause narrowing of the intervertebral foramina, indirectly irritating the nerve root.”
“The increased mechanical tension that shortened muscles generates hastens wear and tear because it pulls on degraded collagen that provides the strength of ligaments, tendons, cartilage, and bone. Neuropathy [radiculopathy] expedites degeneration in weight-bearing and activity—stressed parts of the body, causing spondylosis, discogenic disease, and osteoarthritis among others.”
The primary treatment goal is to “relieve shortening” in muscles that irritate the nerve root and perpetuates the pain.
“Invariably, when muscle shortening is relieved, pain, whether in muscle, tendon, or joint, is alleviated.”
Dr. Gunn’s contribution to the understanding of trigger points and myofascial pain syndromes are important. For example, it is known that the tissue primarily responsible for chronic low back pain is the annulus of the intervertebral disc (15). The tissue primarily responsible for chronic neck pain is the facet joint capsules (16, 17). Dr. Gunn explains how muscle shortening can place pain-producing mechanical stress on joints, capsules, tendons, etc., and how relieving muscle shortening reduces these stresses and their genesis of pain. Thus, trigger point/myofascial therapy not only alleviates muscle pain, but also reduces stress on other generators of pain as well.
Dr. Gunn also adds to the arsenal of ways to effectively address the trigger point and shortened muscle. Much of his book describes the effectiveness of needle acupuncture. Apparently, insertion of the needle into the trigger point will mechanically release it, and in so doing relax the entire muscle.
Dr. Gunn also talks about the value of low-level laser therapy to abort the trigger point. Physiologically, a muscle needs adenosine triphosphate (ATP) to contract. Ironically, a muscle also needs ATP to relax. As noted above, a contracted muscle compromises its own blood supply, reducing the availability of substrates required to make sufficient levels of ATP to relax. Low-level laser therapy works by improving the flow of electrons in the inner membrane of the mitochondria, sharply increasing levels of ATP. The increased ATP so generated allows contracted muscle fibers to relax, including the trigger point, the taught fibers, and the muscle as a whole. Dr. Gunn notes the following:
“Low level laser therapy uses low energy lasers in order to achieve therapeutic effects.”
“LLLT is safe to use: photo-energy emissions are low and treatment is painless, aseptic, and non-thermal.”
“There are no known side effects. There has been no report of eye injury from low-level laser, although care must be taken not to stare into the probe.”
“LLLT has anti-inflammatory and analgesic properties; it accelerates the wound healing process.”
“LLLT is useful in myofascial pain and works well for conditions such as epicondylitis, TMJ dysfunction, pain in the neck, herpes simplex, herpes zoster and post-zoster neuralgia, rotator cuff syndrome (frozen shoulder), carpal tunnel syndrome, acute low back pain, sprain and post-traumatic swelling (hematoma).”
“Laser therapy, with the benefit of painless healing, is widely used.”
•••••••••
The Contributions of David Hubbard, MD
David R. Hubbard, MD, is from the Department of Neurosciences, University of California, San Diego (my alma mater, before chiropractic college). In 1993 he co-wrote an article in the journal Spinetitled (19):
Myofascial Trigger Points Show Spontaneous Needle EMG Activity
Dr. Hubbard notes that trigger points are a common cause of chronic muscle pain. He credits Janet Travell, MD, as the person who first described the trigger pointin 1942, in the Journal of the American Medical Association (6). The purpose of his article was to determine the underlying pathophysiology of the trigger point.
Dr. Hubbard and colleague inserted needle EMG leads into the trigger points of 62 people. On all subjects, they noted spontaneous contractual activity of the trigger point muscle. In some of the subjects they left the needle in place for as long as 50 consecutive minutes, noting a constant contraction of the muscle tissues. Needles inserted into non-trigger point muscle tissue showed no spontaneous electrical activity. If the needle was slightly moved away from the trigger point, in any direction, by as little as a millimeter, the spontaneous electrical activity immediately ceased.
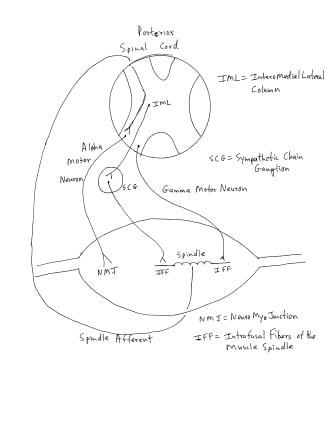
Dr. Hubbard and colleague explain how the intrafusal muscle fiber of the muscle spindle is innervated by the sympathetic nervous system (see drawing). Segmental or regional increases in sympathetic activity would cause a contraction of the small intrafusal muscle of the muscle spindle, which increases the firing of the muscle spindle afferents. Increased muscle spindle afferents into the spinal cord communicate and excite the alpha motor neuron, causing the muscle to contract and shorten. This contraction increases muscle tone, reduces range of motion, and if prolonged, makes the muscle sore and painful. These authors believe that sympathetically stimulated muscle spindle intrafusal fiber contraction “causes an involuntary low-grade but symptomatic muscle tension.” [see drawing]
In supporting evidence for their model, these authors note that in animal studies, sympathetic nerve stimulation causes an increase in tonic muscle tension. Cutting the sympathetic nerves, or administrating sympathetic nerve blocking drugs, immediately inhibits the increase in tonic muscle tension. Dr. Hubbard and colleague state:
“Sympathetic activity explains the autonomic symptoms associated with trigger points and provides a mechanism by which local injury and nociception causes local tension, and by which emotional factors cause widespread tension and pain.”
In short, these authors believe that the trigger point isthe sympathetically contracted intrafusal muscle fibers of the muscle spindle.
It is well established that chiropractic spinal adjusting inhibits segmental/regional increases in sympathetic discharge (20, 21, 22, 23). This is a plausible explanation for the observed improvement in trigger points and myofascial problems following chiropractic spinal adjusting. Chiropractic adjusting, in part, inhibits sympathetic tone, relaxes the intrafusal muscle fibers of the muscle spindle, reduces spindle afferent discharge, reduces muscle tone, improves the range of motion, reducing inflammation and pain.
•••••••••
Perpetuating Factors Back To Dr. Travell
Despite the biological plausibility of her trigger point model, Dr. Travell ran into difficult cases. As stated by her friend, colleague, and co-author Dr. David Simons, Dr. Travell “looked under every physical and medical stone imaginable until she found why that patient had failed to respond to treatment as expected.”(9) She discovered that patients often had one or more of “perpetuating factors.” These perpetuating factors were usually structural inadequacies. The two most common were:
1) A difference in the length of the lower limbs.
2) A long second metatarsal or a short first metatarsal (Morton’s Toe).
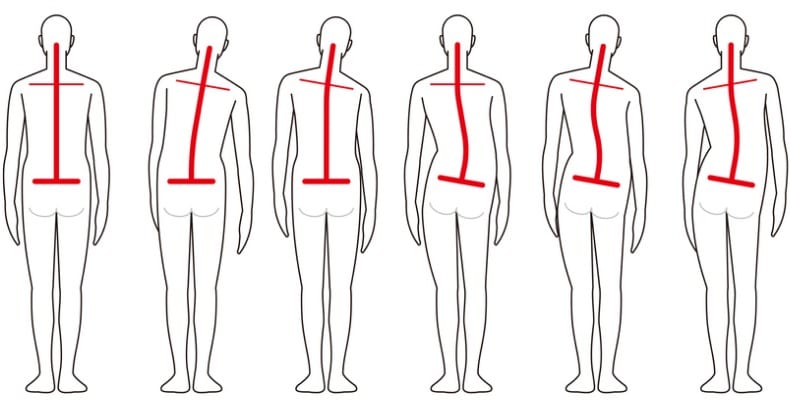
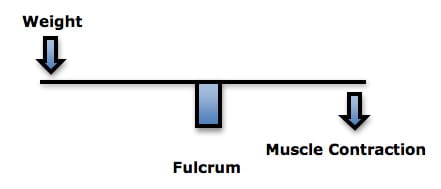
It has been documented since 1946 that about 75% of people have legs of unequal lengths, and that about a third of people have leg length differences that can perpetuate trigger points. As a rule, the sacrum is lower on the side of the short leg (see drawing). The spinal column initially tilts towards the short leg, then compensates back to the midline as a consequence of chronic contraction of the quatratus lumborum muscle. According to Dr. Travell, the resulting trigger points in the quadratus lumborum muscle is a very common but frequently overlooked cause of chronic low back pain (13).
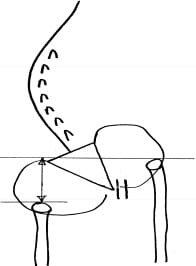
The Morton’s Toe was described by American orthopedic surgeon Dudley J. Morton, MD, from Yale, in 1927 (25). Dr. Morton noted that people suffered from a variety of chronic pain syndromes when they had a long second metatarsal or a short first metatarsal (which he termed Morton’s Toe). This common anatomic variant would alter the normal weight-bearing function of the foot, causing a compensatory pronation. Travell observed that this would lower the pelvis on that side, creating the identical trigger points as a leg length inequality.
Dr. Travell notes that the solution is a proper heal lift and an shoe orthotic that re-establishes foot mechanics and weight-bearing, usually by correcting the pronation. She notes that other causes of foot pronation can and should be similarly addressed with an orthotic.
Dr. Travell also “discovered that one of [Senator] Kennedy’s legs was shorter than the other and made heel lifts for all of his left shoes to counter that additional source of stress on his back.” “Dr. Travell had a workbench in her office and made lifts for both patients and family members. ‘One of the first things I did for him [Kennedy] was to institute a heel lift—a correction for the difference in leg length’.”(10)
References
- pain-education.com/dr-travell.html; A Tribute to Dr. Janet Travell; accessed December 11, 2013.
- Lacayo R; How Sick Was J.F.K.?; TIME; November24, 2002.
- Altman LK, Purdum TS; In J.F.K. File, Hidden Illness, Pain and Pills; The New York Times; November 17, 2002.
- Dallek R; The Medical Ordeals of JFK; The Atlantic; December 2002.
- Wilson V; Janet G. Travell, MD: A Daughter’s Recollection; Texas Heart Institute Journal; 2003; Vol. 30; No. 1; pp. 8–12.
- Travell J, Rinzler S, Herman M; Pain and disability of the Shoulder and Arm: Treatment by Intramuscular Infiltration with Procaine Hydrochloride; Journal of the American Medical Association; October 10,1942; Vol. 120; No. 6; pp. 417-422.
- Travell J, Rinzler SH; Relief of cardiac pain by local block of somatic trigger areas. Proc Soc Exp Biol Med 1946;63:480–2.
- Rinzler SH, Travell JG. Therapy directed at the somatic component of cardiac pain. Am Heart J 1948;35:248–68.
- Simons DG; Cardiology and Myofascial Trigger Points: Janet G. Travell’s Contribution; Texas Heart Institute Journal; 2003; 30; No. 1; pp. 3–7.
- Bagg JE; The President’s Physician; Texas Heart Institute Journal; 2003; 30; No. 1pp. 1–2.
- Gunn CC; The Gunn Approach to the Treatment of Chronic Pain:Intramuscular Stimulation for Myofascial Pain of Radiculopthic Origin; Churchill Livingston, 1996.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual; New York: Williams & Wilkins, 1983.
- Travell J, Simons D; Myofascial pain and dysfunction, the trigger point manual: THE LOWER EXTREMITIES; New York: Williams & Wilkins, 1992.
- Simons D, Travell J; Travell & Simons’,Myofascial pain and dysfunction, the trigger point manual: Volume 1, Upper Half of Body; Baltimore: Williams & Wilkins, 1999.
- Kuslich S, Ulstrom C, Michael C; The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anesthesia; Orthopedic Clinics of North America, Vol. 22, No. 2, April 1991, pp. 181-187.
- Bogduk N, Aprill C; On the nature of neck pain, discography and cervical zygapophysial joint blocks; Pain; August 1993;54(2):213-7.
- Bogduk N; On Cervical Zygapophysial Joint Pain After Whiplash; Spine; December 1, 2011; Volume 36, Number 25S, pp S194–S199.
- Cailliet R; Soft Tissue Pain and Disability; 3rdEdition; F A Davis Company, 1996.
- Hubbard DR, Berkoff GM; Myofascial Trigger Points Show Spontaneous Needle EMG Activity; Spine; October 1993; Vol. 18; No. 13; pp. 1803-1807.
- Korr IM; The spinal cord as organizer of disease processes: III. Hyperactivity of sympathetic innervation as a common factor in disease; December 1979;79(4):232-237.
- Budgell B, Hirano F; Innocuous mechanical stimulation of the neck and alterations in heart-rate variability in healthy young adults; Autonomic Neuroscience; 2001 Aug 13;91(1-2):96-99.
- Koch LE, Koch H, Graumann-Brunt S, Stolle D, Ramirez JM; Saternus KS; Heart rate changes in response to mild mechanical irritation of the high cervical spinal cord region in infants; Forensic Science International; Volume 128, Issue 3, August 28, 2002, Pages 168-176.
- Ogura T, Tashiro T, Masud M, et. al; Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain; Alternative Therapies Health Medicine; Nov-Dec 2011;Vol. 17; No. 6; pp. 12-7.
- Rush WA, Steiner HA; A Study of Lower Extremity Length Inequality; American Journal of Roentgenology and Radium Therapy; Vol. 51, No. 5, November 1946, 616-623.
- Morton DJ; METATARSUS ATAVICUS: The Identification of a Distinctive Type of FootDisorder;J Bone Joint Surg Am, 1927 Jul 01;9(3):531-544.