QUESTION:
If a tree falls in the woods when no one is present, does it make a sound?
COMMON RESPONSE LAY PERSON:
Yes
COMMON RESPONSE MEDICAL PROFESSIONAL:
No
DISCUSSION:
All perceptions are cortical. The perception of sound is a cortical event. If no one is present, there is no cortex present, and therefore there is no sound. When a tree falls in the woods it creates a physical phenomenon that is capable of creating the perception of sound in the cortical brain; but without the cortical brain being present, there is no sound.
EXCHANGE:
From the movie, THE MATRIX:
QUESTION by Morpheus:
What is real, Neo?
RESPONSE by Neo:
I do not know.
RESPONSE by Morpheus:
Real is an electrical signal interpreted by your brain.
QUESTION:
What is pain?
RESPONSE (Murphy):
Pain is an electrical signal interpreted by your brain.
DISCUSSION:
Pain, like sound (and sight, taste, smell, hot/cold, etc.), is a cortical event. It is an electrical signal in one’s brain.
•••••••••
Chiropractors thrive in the treatment and management of regional musculoskeletal pain complaints. The clinical efficacy of chiropractic in the treatment and management of musculoskeletal pain syndromes is no longer questioned. As examples, in 1985, orthopedic surgeon W. H. Kirkaldy-Willis states (1):
“Spinal manipulation, one of the oldest forms of therapy for back pain, has mostly been practiced outside of the medical profession.”
“Over the past decade, there has been an escalation of clinical and basic science research on manipulative therapy, which has shown that there is a scientific basis for the treatment of back pain by manipulation.”
A 2011 study authored by Ogura and 8 additional researchers, all with the credentials of MD/PhD, states (2):
“Chiropractic spinal manipulation is an alternative treatment or back pain.”
“Research on chiropractic spinal manipulation has been extensively performed worldwide, and its efficacy on musculoskeletal symptoms has been well documented.”
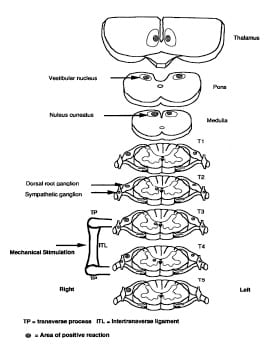
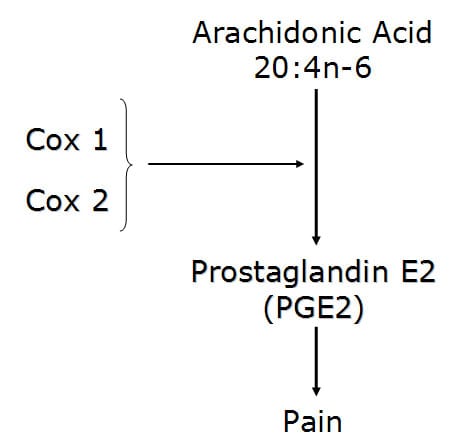
The physiological explanations as to the mechanisms whereby chiropractic adjusting (directionally specific manipulation) influences pain syndromes (an electrical signal in the brain) tend to fall primarily into two categories:
- Altering inflammation [The Inflammatory Cascade: reducing excitation]
- Closing the pain gate [The Pain Gate: increasing inhibition]
The Inflammatory Cascade
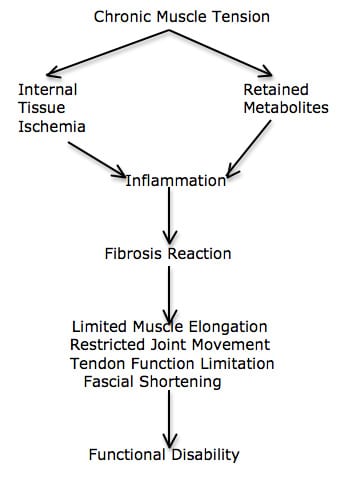
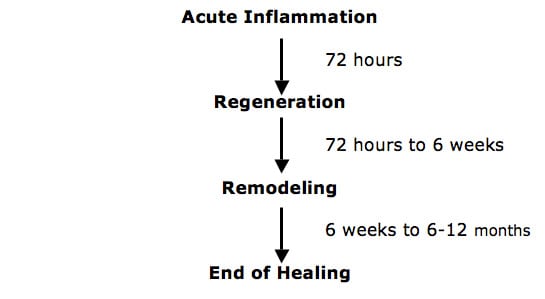
- Tissue trauma or repetitive strain injury initiate an inflammatory response (3, 4, 5).
- Inflammation alters the electrical threshold of the pain afferents (6, 7). Inflamed tissue more readily initiates the neurological electrical signal that in turn creates the pain perceiving electrical signal in the brain. Sunburned skin is much closer to pain threshold than non-sunburned skin when exposed to an environmental stimulus, such as touching or rubbing.
- As a rule, the resolution of inflammation in the body is fibrotic scar tissue (3, 8, 9, 10, 11, 12, 13, 14, 15, 16).
- Fibrous scar tissue is capable of maintaining an inflammatory response, chronically altering the threshold of the pain afferent system, and therefore chronically initiating a chronic pain electrical signal in the brain (3).
- Tension, controlled motion (chiropractic adjustment), remodels the fibrous scar tissue; this orients the tissues along the lines of stress and strain (3, 4, 9, 10, 11, 12, 13, 14, 15, 16, 17). The fibrous scar tissue will no longer harbor an inflammatory response. In addition, the improved motion will further disperse the accumulation of inflammatory exudates. Reduced inflammation reduces the pain electrical signal in the cortical brain.
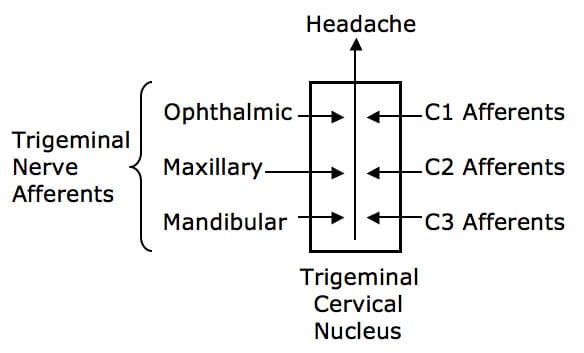
The Pain Gate
Melzack and Wall’s Gate Control Theory of Pain was originally published in the journal Brain in 1962, and later updated and published in the journal Science in 1965. Ronald Melzack, PhD, is a Canadian psychologist. Patrick Wall, MD (d. 2001), was a British neuroscientist and pain expert, as well as the first editor of the journal Pain. An oversimplified explanation of their Gate Control Theory of Pain is that the pain electrical signal to the cortical brain (small diameter afferents) can be inhibited by non-painful electrical signals arising from other sensory afferents (large diameter afferents). Representative reference book comments include:
The perception of pain is dependent upon the balance of activity in large (mechanoreceptor) and small (nociceptive) afferents. (18)
If large myelinated fibers (mechanoreceptors) were selectively stimulated, then normal “balance” of activity between large (mechanoreceptor) and small (nociceptive) fibers would be restored and the pain would be relieved. (18)
“Pain is not simply a direct product of the activity of nociceptive afferent fibers but is regulated by activity in other myelinated afferents that are not directly concerned with the transmission of nociceptive information.” (19)
“The idea that pain results from the balance of activity in nociceptive and non-nociceptive afferents was formulated in the 1960s and was called the gate control theory.” (19)
“Simply put, non-nociceptive afferents ‘close’ and nociceptive afferents ‘open’ a gate to the central transmission of noxious input.” (19)
“The balance of activity in small- and large-diameter fibers is important in pain transmission…” (19)
Melzack and Wall’s Gate Control Theory of Pain was reviewed and confirmed in 2002 in the British Journal of Anaesthesia in an article titled (20):
Gate Control Theory of Pain Stands the Test of Time
This article reiterates that the Gate Theory “has stood the test of time.” The electrical transmission and perception of pain is subject to modulation by non-nociceptive neurological electrical signals. These non-nociceptive neurological electrical signals emanate from large diameter nerve fibers, such as mechanoreceptors. Consequently, the author notes that pain can be modulated through 2 mechanisms (as noted above):
- Reducing excitation. This approach is commonly achieved by reducing inflammation.
- Increasing Inhibition. This approach is commonly achieved by improving mechanical function and mechanical afferentation, firing inhibitory large diameter mechanoreceptors.
The application of chiropractic spinal adjusting for pain control using
Melzack and Wall’s Gate Control Theory of Pain was first done by Canadian orthopedic surgeon Kirkaldy-Willis in 1985 (1). Dr. Kirdaldy-Willis notes:
“Spinal manipulation is essentially an assisted passive motion applied to the spinal apophyseal and sacroiliac joints.”
Melzack and Wall proposed the Gate Theory of Pain in 1965, and this theory has “withstood rigorous scientific scrutiny.”
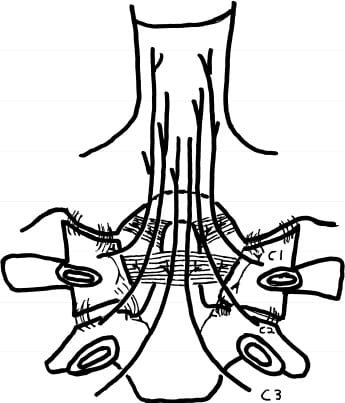
“The central transmission of pain can be blocked by increased proprioceptive input.” Pain is facilitated by “lack of proprioceptive input.” This is why it is important for “early mobilization to control pain after musculoskeletal injury.”
The facet capsules are densely populated with mechanoreceptors. “Increased proprioceptive input in the form of spinal mobility tends to decrease the central transmission of pain from adjacent spinal structures by closing the gate. Any therapy which induces motion into articular structures will help inhibit pain transmission by this means.”
Stretching of facet joint capsules will fire capsular mechanoreceptors which will reflexly “inhibit facilitated motoneuron pools” which are responsible for the muscle spasms that commonly accompany low back pain.
In chronic cases, there is a shortening of periarticular connective tissues and intra-articular adhesions may form; manipulations [adjustments] can stretch or break these adhesions.
“In most cases of chronic low back pain, there is an initial increase in symptoms after the first few manipulations [probably as a result of breaking adhesions]. In almost all cases, however, this increase in pain is temporary and can be easily controlled by local application of ice.”
“However, the gain in mobility must be maintained during this period to prevent further adhesion formation.”
These patients were given a “two or three week regimen of daily spinal manipulations by an experienced chiropractor.”
“No patients were made worse by the manipulation, yet many experienced an increase in pain during the first week of treatment. Patients undergoing manipulative treatment must therefore be reassured that the initial discomfort is only temporary.”
“In our experience, anything less than two weeks of daily manipulation is inadequate for chronic low back pain patients.”
•••••••••
Chiropractors pride themselves on their abilities to treat and manage regional musculoskeletal pain complaints. It is understood that many different tissues can initiate the pain electrical signal to the brain, including the intervertebral disc, joint capsules, tendons, muscles, myofascia, and more. Consequently, chiropractic management of regional musculoskeletal pain complaints often involve several simultaneous approaches. These approaches tend to adhere to the concepts noted above:
1) Altering inflammation, reducing excitation:
Management might include local applications of ice, low level laser therapy, pulsed ultrasound, etc.
Local passive motions, soft tissue friction techniques, specific exercises, and chiropractic adjusting may remodel fibrotic scar tissue, dispersing the accumulation of algogenic inflammatory exudates that are altering the electrical threshold of the local pain afferents.
2) Closing the pain gate, increasing inhibition:
There is evidence that chiropractic adjusting can remodel peri-articular fibrosis and rupture intra-articular fibrotic adhesions (21). As noted by Kirkaldy-Willis above, this would improve motion, mechanoreception, and proprioception, “closing” the pain gate, or increasing inhibition. Also as noted by Kirkaldy-Willis, these fibrotic problems tend to reform, denying the long-term benefits that both patients and chiropractors strive to obtain. Consequently, chronic pain patients may respond best to daily manipulation during the initial 2 weeks of management.
•••••••••
Problems
Chiropractors are noted for their treatment and management of patients with chronic pain problems. On occasion, or perhaps more frequently, the patient’s pain is not primarily local or regional, but rather is systemic. There are a number of known factors that can systemically alter the threshold of the pain afferents. These individuals perceive the electrical signal of pain following trivial mechanical stimuli, stimuli that under normal circumstances wild not initiate that pain electrical signal. Common terminology for such individuals is “the patient is systemically too close to nociceptive excitation threshold.”
There are undoubtedly many biological reasons for a patient to be systemically to close to nociceptive excitation threshold. Three common and well-documented reasons are discussed below. Chiropractors often assess these factors in their pain patients as a component of history and/or blood work, and chiropractors often advise their patients in the management of their finding.
•••••••••
Jill is a 30-year old female with chronic systemic pain. She has been suffering from chronic systemic pain for about a decade. For help, she has tried pharmacology, massage, yoga, Pilates, acupuncture, physical therapy, exercise, psychotherapy, and chiropractic. None of these approaches has made much of a difference. She is currently taking 6 different medicines for her pain, even though “they do not seem to be helping very much.”
•••••••••
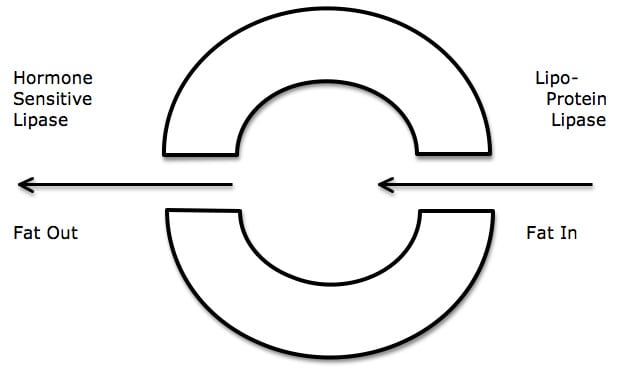
Omega-6/Omega-3 Ratio
In all of our chronic pain patients, whether their pain is local, regional, or systemic, we find great value in assessing their systemic inflammation profile. To do this we use the protocols of biochemist Barry Sears, PhD (22, 23). Dr. Sears and many others contend that systemic inflammation is primarily controlled by the balance of inflammatory v. anti-inflammatory eicosanoid hormones (24, 25, 26). Eicosanoid hormones are made from 20-carbon long unsaturated fatty acids. Dr. Sears stresses that the best test for systemic inflammation is the ratio of the omega-6 fatty acid arachidonic acid (AA) to the omega-3 fatty acid eicosapentaenoic acid (EPA). He states (23):
“The AA/EPA ratio will tell you the extent
of silent inflammation in the body.”
Based upon the writings of Dr. Sears and many others, we target an
Arachidonic acid (AA) omega-6 / Eicosapentaenoic Acid (EPA) omega-3 ratio of 1.5-4 / 1. A ratio > 10 / 1 is very problematic and is indicative of systemic inflammation. Sadly, because of contemporary widespread use of corn, soybean, and other omega-6 vegetable oils, the average American ratio now stands at about 25 / 1 (6, 27). This means that the average American is extremely systemically inflamed and prone to systemic pain syndromes. Recent evidence from the Institute of Medicine claims that now 116 million Americans suffer from chronic daily pain syndromes (28). We obtain an accurate systemic inflammation profile using a simple finger-prick blood analysis.
•••••••••
Jill’s AA / EPA ratio was 15 / 1; this is clearly significantly pro-inflammatory. We immediately put Jill on 3,000 mg/day of EPA + DHA purified fish oil supplements, with a compliment of anti-oxidants to reduce lipid peroxidation of the double bonds.
•••••••••
Vitamin D
Using the key words “vitamin D AND chronic pain” in a pubmed search of the national Library of Medicine (March 11, 2013) will call up 208 articles. In 2008, James Dowd, MD, authored a book titled The Vitamin D Cure (29). Dr. Dowd notes that adequate vitamin D supplementation can eliminate chronic back pain symptoms in nearly all patients, stating:
“Research tells us that a lack of vitamin D makes us ache. Symptoms that point to vitamin D deficiency are muscle spasms, bone pain, and joint pain.”
“Doctors often mistake vitamin D deficiencies for fibromyalgia, rheumatoid arthritis, and lupus.”
“Because I’m a rheumatologist, people come to me because they want solutions for the pain they’re experiencing in their joints, tendons, ligaments, muscles, and bones. They typically have at least one disease involving muscles, ligaments, joints, and bones, but all of the aches and pains they have are actually connected to their vitamin D levels and what they eat.”
“Those who took vitamin D supplements saw dramatic resolution of pain, muscle fatigue and muscle cramps.”
The world’s leading authority on vitamin D is Michael F. Holick, PhD, MD. Dr. Holick is a professor at Boston University Medical Center. A search of the National Library of Medicine using the pubmed search engine found 380 articles using the key words “holick mf AND vitamin d”. Dr. Holick is the discoverer of the active form of vitamin D (1,25, dihydroxy vitamin D).
In his 2010 book titled The Vitamin D Solution; A 3-Step Strategy to Cure Our Most Common Health Problems, Dr. Holick notes that 93% of those suffering from nonspecific muscular and skeletal aches and pains are shown to be vitamin D deficient (30). Numerous other recent publications agree with Dr. Holick (31, 32, 33, 34, 35, 36, 37, 38). A central theme among these authors is that low levels of vitamin D are linked to inflammation, and as noted above, inflammation alters the thresholds of the pain afferent system.
In 2010, Joseph Pizzorno, ND, the Editor in Chief of the journal
Integrative Medicine, published an editorial in his journal titled: What We Have Learned About Vitamin D Dosing? (39) Dr. Pizzorno believes that the minimum blood levels of vitamin D [25(OH)D3] is 32 ng/ml; the optimal level is 50-70 ng/ml. He recommends that when vitamin D levels are below 32 ng/ml, a loading dose of supplemental vitamin D3 of about 20,000 IU/day for 3–6 months with a maintenance dose of 5,000
IU/day is warranted.
We recommend that all chronic pain patients should have their 25-hydroxy vitamin D levels checked. We obtain an accurate 25-hydroxy vitamin D levels using another simple finger-prick blood analysis. If a patient’s 25-hydroxy vitamin D levels are below 50 ng/ml, and especially if they are below 30 mg/ml, the patient needs more UVB sun exposure without sunscreen, or they need to supplement.
•••••••••
Jill’s 25-hydroxy vitamin D was 17 ng/ml; this is clearly too low and significantly pro-inflammatory. We immediately put Jill on 20,000 IU/day of vitamin D3 with the intention of following Dr. Pizzorno’s protocol above.
•••••••••
Glutamate and Aspartate
An excess of the brain’s principle excitatory neurotransmitters can enhance the pain electrical signal in the brain. The brain’s 2 principle excitatory neurotransmitters are glutamate and aspartate. Both glutamate and aspartate are amino acids. Both glutamate and aspartate are commonly isolated and added to foods as taste enhancers (exciters). Both glutamate and aspartate use the N-methyl-D-aspartate (NMDA) receptor.
Aspartate is half of the artificial sweetener aspartame. Glutamate is ubiquitous in packaged foods, often in the salt form MSG (monosodium glutamate). Glutamate in food is often hidden, using names like (40):
HIDDEN SOURCES OF MSG
The glutamate manufacturers and the processed food industries are always on a quest to disguise MSG added to food. Below is a partial list of the most common names for disguised MSG.
Additives that always contain MSG:
- Monosodium Glutamate
- Hydrolyzed Protein
- Plant Protein Extract
- Calcium Caseinate
- Textured Protein
- Hydrolyzed Oat Flour
- Hydrolyzed Vegetable Protein
- Hydrolyzed Plant Protein
- Sodium Caseinate
- Yeast Extract
- Autolyzed Yeast
Additives that frequently contain MSG:
- Malt Extract
- Malt Flavoring
- Bouillon
- Broth
- Stock
- Flavoring
- Natural Flavoring
- Natural Beef or Chicken Flavoring
- Seasoning
- Spices
Additives that may contain MSG or excitotoxins:
- Carrageenan Enzymes
- Soy Protein Concentrate Soy Protein Isolate
- Whey Protein Concentrate
In 2002, Dickenson (20) clearly notes that glutamate is involved in chronic pain sensization. Recent studies (2012) continue to confirm that dietary glutamate (or aspartate) are involved in chronic pain syndromes (41, 42).
In 2001, Jerry D. Smith and colleagues took a group of chronic pain suffers and purposefully removed all sources of isolated glutamate and aspartame form their diets. Within 4 months, all study subjects reported complete resolution of their pain symptoms. Additionally, reintroduction of isolated glutamate or aspartame into any of their diets immediately resurrected their pain symptoms.
With chronic pain patients, we routinely assess consumption of glutamate (often hidden) and aspartame. We advocate complete avoidance for the next 4 months.
•••••••••
Jill’s consumption of glutamate was probably average. However, history revealed that she was consuming 6 diet sodas (sweetened with aspartame) daily. We immediately had her stop all diet soda consumption, cold turkey.
•••••••••
As clinicians and not researchers, our approach to the management of Jill’s chronic pain was multifaceted, including:
- Chiropractic adjusting of dysfunctional joints.
- Spinal exercises, beginning weight training, and graded walking.
- Supplemental fish oil omega-3 fatty acids plus antioxidants.
- Supplemental vitamin D3.
- Reduction of dietary glutamate and elimination of all aspartame.
Jill’s chronic pain was markedly improved after one month of this regime, and she was pain free at the 4 month revaluation.
REFERENCES
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985, Vol. 31, pp. 535-540.
- Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, Itoh M, Fukuda H, Yanai K; Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain; Alternative Therapies Health Medicine; Nov-Dec 2011;Vol. 17; No. 6; pp. 12-7.
- Cyriax, James; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions, Bailliere Tindall, Volume 1, eighth edition, 1982.
- Roy, Steven; Irvin, Richard; Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation, Prentice-Hall, 1983.
- Maroon JC, Bost JW, Maroon A; Natural anti-inflammatory agents for pain relief; Surgical Neurological International; Dec. 2010; Vol. 13; No. 1.
- Boswell M, Cole BE, editors; American Academy of Pain Management: Weiner’s Pain Management: A Practical Guide for Clinicians; Seventh Edition, 2006, pp. 584-585.
- Omoigui S; The biochemical origin of pain: The origin of all pain is inflammation and the inflammatory response: Inflammatory profile of pain syndromes; Medical Hypothesis; 2007, Vol. 69, pp. 1169–1178.
- Guyton, Arthur, Textbook of Medical Physiology, Saunders, 1986.
- Cohen, I. Kelman; Diegelmann, Robert F; Lindbald, William J; Wound Healing, Biochemical & Clinical Aspects, WB Saunders, 1992.
- Melham TJ, Sevier TL, Malnofski MJ, Wilson JK, Helfst RK, Chronic ankle pain and fibrosis successfully treated with a new noninvasive augmented soft tissue mobilization technique (ASTM); Medicine Science Sports Exercise, June 1998; 30(3): 801-4.
- Jonsson H, Cesarini K, Sahlstedt B, Rauschning W; Findings and Outcome in Whiplash-Type Neck Distortions; Spine, Vol. 19, No. 24, December 15, 1994, pp. 2733-2743.
- Hildebrand K, Frank C; Scar Formation and Ligament Healing; Canadian Journal of Surgery; 1998.
- Majno, Guido and Joris, Isabelle; Cells, Tissues, and Disease: Principles of General Pathology, 2004.
- Hildebrand KA, Gallant-Behm CL, Kydd AS, Hart DA; The Basics of Soft Tissue Healing and General Factors that Influence Such Healing; Sports Medicine Arthroscopic Review; 2005.
- Walsh W; Orthopedic Biology and Medicine; Repair and Regeneration of Ligaments, Tendons, and Joint Capsule; Humana Press, 2006.
- Schleip R; Fascia: The Tensional Network of the Human Body; The Scientific and Clinical Applications in Manual and Movement Therapy; 2012.
- Kellett J; Acute soft tissue injuries-a review of the literature; Medicine and Science of Sports and Exercise, American College of Sports Medicine, Vol. 18 No. 5, (1986), pp. 489-500.
- John Nolte, The Human Brain; Mosby Year Book, 1993.
- Eric Kandel, James Schwartz, Thomas Jessell, Principles of Neural Science. McGraw-Hill, 2000.
- Dickenson AH; Gate Control Theory of pain stands the test of time; British Journal of Anaesthesia, Vol. 88, No. 6, June 2002, pp. 755-757.
- Cramer GD, Gregerson DM, Knudsen JT, Hubbard BB, Ustas LM, Cantu JA; The Effects of Side-Posture Positioning and Spinal Adjusting on the Lumbar Z Joints: A Randomized Controlled Trial With Sixty-Four Subjects; Spine, Volume 27, Issue 22, November 15, 2002, pp. 2459-2466.
- Barry Sears; The Omega Zone; Regan Books; 2002.
- Barry Sears; Toxic Fat; Thomas Nelson; 2008.
- Cleland LG, James MJ, Proudman SM; What the prescriber needs to know; Arthritis Res Ther. 2006;8(1):202.
- Goldberg RJ, Katz J; A meta-analysis of the analgesic effects of omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain; Pain; May 2007, 129(1-2), pp. 210-223.
- Maroon JC, Bost JW; Omega-3 Fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain; Surgical Neurology; 65 (April 2006) 326–331.
- Simopoulos AP; Evolutionary Aspects of Diet: The Omega-6/Omega-3 Ratio and the Brain; Molecular Neurobiology; October 2011; Vol. 44; No. 2; pp. 203-15.
- Pho K; Pain Management: Education is Key; USA Today; September 9, 2011, p. 9A.
- Dowd J; The Vitamin D Cure; Wiley, 2008.
- Holick MF; The Vitamin D Solution; A 3-Step Strategy to Cure Our Most Common Health Problems; 2010.
- Schwalfenberg G; Improvement of Chronic Back Pain or Failed Back Surgery with Vitamin D Repletion: A Case Series; Journal of the American Board of Family Medicine; January–February 2009; Vol. 22; No. 1; pp. 69-74.
- Straube S, Andrew Moor R, Derry S, McQuay HJ, Thomas A; Vitamin D and chronic pain; Pain; 2009; 141: pp. 10-13.
- Manson JE; Pain: sex differences and implications for treatment; Metabolism; October 2010, Volume 59, Supplement 1, pp. S16-S20.
- Heidari B, Shirvani JS, Firouzjahi A, Heidari P, Hajian-Tilaki KO; Association between nonspecific skeletal pain and vitamin D deficiency; International Journal of Rheumatic Disease; October 2010; Vol. 13. No. 4; pp. 340-346.
- Bhatty SA, Shaikh NA, Irfan M, Kashif SM, Vaswani AS, Sumbhai A, Gunpat; Vitamin D Deficiency in Fibromyalgia; Journal of the Pakistan Medical Association; November 2010; Vol. 60; No. 11; pp. 949-951.
- Arnson Y, Amital H; Is Vitamin D a New Therapeutic Agent in Auto-inflammatory and Pain Syndromes?; Israeli Medical Association Journal; Vol. 13, April 2011; pp. 234-235.
- Tague SE, Clarke GL, Winter MK, McCarson KE, Wright DE, Smith PG; Vitamin D deficiency Promotes Skeletal Muscle Hypersensitivity and Sensory Hyperinnervation; Journal of Neuroscience; September 2011; Vol. 31; No. 39; pp. 13728-38.
- Kragstrup TW; Vitamin D Supplementation for Patients with Chronic Pain; Scandinavian Journal of Primary Health Care; 2011, 29: pp. 4-5.
- Pizzorno J; What We Have Learned About Vitamin D Dosing?; Integrative Medicine; Vol. 9, No. 1, Feb/Mar 2010.
- Blaylock R; Excitotoxins, The Taste That Kills; Health Press, 1997.
- Ma X, Shi TF, Zhang M, Lu XY, and six more; Modulatory role of glutamic acid on the electrical activities of pain-related neurons in the hippocampal CA3 region; Neuroscience Letters; March 2012; Vol. 513; No. 1; pp. 67-71.
- Holton KF, Taren DL, Thomson CA, Bennett RM; Jones KD; The effect of dietary glutamate on fibromyalgia and irritable bowel symptoms; Clinical Experimental Rheumatology; Nov-Dec 2012; 30(6 Suppl 74); pp. 10-7.
- Smith JD, Terpening CM, Schmidt SOF, Gums JG; Relief of Fibromyalgia Symptoms Following Discontinuation of Dietary Excitotoxins; The Annals of Pharmacotherapy: June 2001; Vol. 35, No. 6, pp. 702–706.

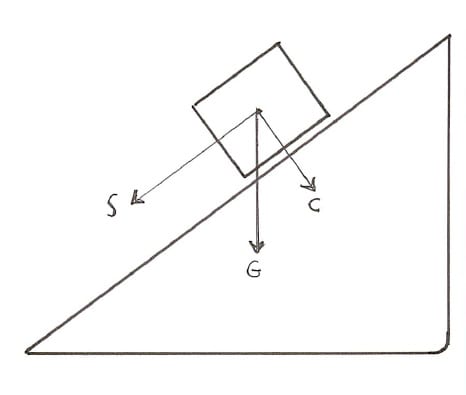




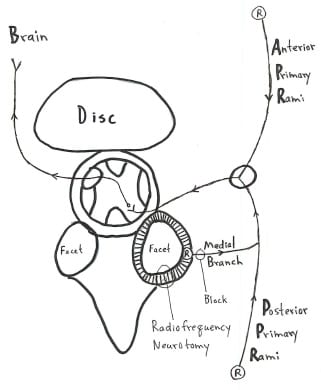

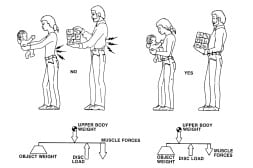
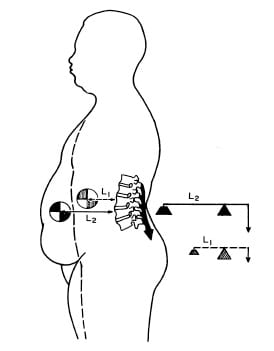
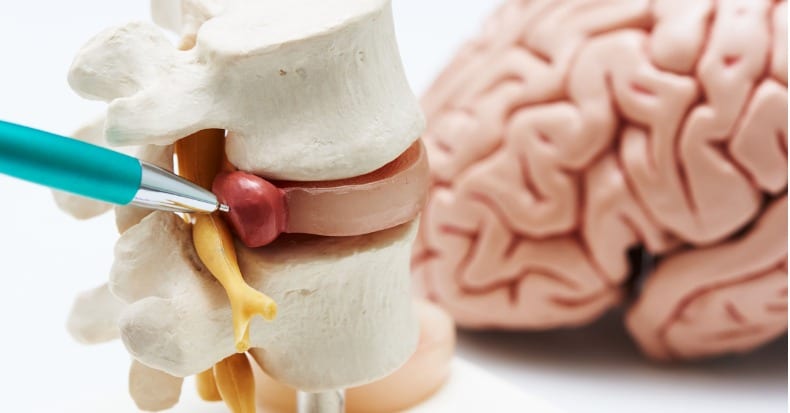
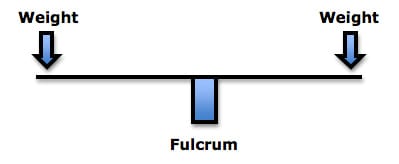 The fulcrum of a first class lever is the place where the force is the greatest: if excessively heavy objects are placed on both ends of the teeter-totter, it will break in the middle, at the fulcrum. In the spine, the fulcrum of the first class lever is the vertebra. Approximately 60% of weight is born by the vertebral body/intervertebral disc complex, and the other 40% is shared between the two facet joints. This means that when the first class lever of upright posture is altered, for any reason, there is an increased mechanical load born by the fulcrum, i.e. the spinal intervertebral discs and facet joints. Such increased mechanical loads accelerate degenerative joint disease (1, 3). In their 1990 book Clinical Biomechanics of the Spine (2), White and Panjabi state:
The fulcrum of a first class lever is the place where the force is the greatest: if excessively heavy objects are placed on both ends of the teeter-totter, it will break in the middle, at the fulcrum. In the spine, the fulcrum of the first class lever is the vertebra. Approximately 60% of weight is born by the vertebral body/intervertebral disc complex, and the other 40% is shared between the two facet joints. This means that when the first class lever of upright posture is altered, for any reason, there is an increased mechanical load born by the fulcrum, i.e. the spinal intervertebral discs and facet joints. Such increased mechanical loads accelerate degenerative joint disease (1, 3). In their 1990 book Clinical Biomechanics of the Spine (2), White and Panjabi state: