Historical Context
Alfred Bernhard Nobel was a Swedish chemist, engineer, inventor, and businessman. He was born in 1833 and died in 1896. He held 355 patents in his lifetime, the most notorious of which was for dynamite. Dynamite used the explosive power of nitroglycerin. Nobel patented dynamite in 1867.
Nobel amassed a fortune during his lifetime. In his will, he bequeathed most of his fortune to establish five prizes which became known as “Nobel Prizes.” These prizes were to be awarded for contributions that have conferred the greatest benefit to mankind in the areas of:
- Physics
- Chemistry
- Physiology or Medicine
- Literature
- Peace
Today, Nobel Prizes are widely regarded as the most prestigious awards available in their respective fields.
The first Nobel Prizes were awarded in 1901. In 1968 a Nobel Prize in Economics was added.
The Basic Chiropractic Premise
Manipulation and chiropractic-type of healthcare procedures have a long history (1, 2, 3). For at least 2,500 years, spinal manipulation has been practiced in many parts of the world, primarily to treat musculoskeletal disorders. Ancient evidence for the application of spinal manipulation has been documented in:
- Bohemian (Czechoslovakia)
- China
- Egypt
- England
- Finland
- Greece
- India
- Japan
- Latin America
- Norway
- Russia
- Wales
In 2007, a study published in The Journal of Manual & Manipulative Therapy notes (3):
“Manipulative therapy has known a parallel development throughout many parts of the world. The earliest historical reference to the practice of manipulative therapy in Europe dates back to 400 BCE.”
“Historically, manipulation can trace its origins from parallel developments in many parts of the world where it was used to treat a variety of musculoskeletal conditions, including spinal disorders.”
“It is acknowledged that spinal manipulation is and was widely practiced in many cultures and often in remote world communities such as by the Balinese of Indonesia, the Lomi-Lomi of Hawaii, in areas of Japan, China and India, by the shamans of Central Asia, by sabodors in Mexico, by bone setters of Nepal as well as by bone setters in Russia and Norway.”
“Historical reference to Greece provides the first direct evidence of the practice of spinal manipulation.”
“Hippocrates (460–385 BCE), who is often referred to as the father of medicine, was the first physician to describe spinal manipulative techniques.”
“Claudius Galen (131–202 CE), a noted Roman surgeon, provided evidence of manipulation including the acts of standing or walking on the dysfunctional spinal region.”
“Avicenna (also known as the doctor of doctors) from Baghdad (980–1037 CE) included descriptions of Hippocrates’ techniques in his medical text The Book of Healing.”
In her 1990 book, Mutant Message Down Under, Marlo Morgan chronicles the journey of a middle-aged, white, American woman with a group of 62 desert Aborigines across the continent of Australia (1). Morgan chronicled a cultural habit, estimated to be millennia old, at the end of each day’s nomadic journey: members of the group spinal manipulating each other.
For most of this history, the practitioners of manipulation were known as bonesetters (3). In the United States, in the year 1874, physician Andrew Taylor Still established the American Osteopathic College in Kirksville, Missouri. By the time of his death in 1917, 3,000 Doctors of Osteopathy had graduated from his school.
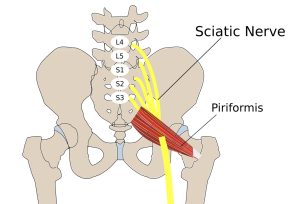
In 1895, “natural healer” Daniel David (DD) Palmer reasoned that when a vertebra was out of alignment, it caused pressure on nerves. In 1897, Palmer opened his first college, The Palmer College of Cure, now known as Palmer College of Chiropractic, Davenport, Iowa (3).
Today, there are 18 chiropractic colleges in the United States and many more throughout the world (4). Some of the chiropractic colleges are Universities that grant academic degrees in addition to the Doctor of Chiropractic degree (DC). Others only grant Doctor of Chiropractic degrees.
In the 1970s, the federal government took control of chiropractic education in the U.S. The United States Department of Education oversees chiropractic education by recognizing the Council for Chiropractic Education (CCE) (4):
“CCE maintains recognition by the United States Department of Education as the national accrediting body for Doctor of Chiropractic Programs and chiropractic solitary purpose institutions of higher education.”
All 18 of the chiropractic colleges in the United States are accredited by the Council for Chiropractic Education.
In the United States, the licensure of chiropractors is controlled by the individual states, and all 50 U.S. states officially license chiropractors, allowing them to practice with their Doctor of Chiropractic degree (DC). Chiropractors are considered to be primary health care providers, which means (in part) that the public may choose chiropractic care without requiring a referral from another health care provider.
As a result of their education and examination procedures, chiropractors are legally allowed to provide a number of services to their patients. These include physical therapy, exercise, tissue work, dietary advice, use of supplements, the taking of and the interpretation of x-rays, etc. But the central core of chiropractic clinical practice is the use of mechanical care, and the primary form of mechanical care is specific line-of-drive manipulation (the chiropractic adjustment).
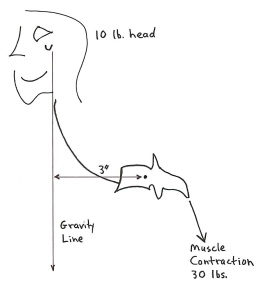
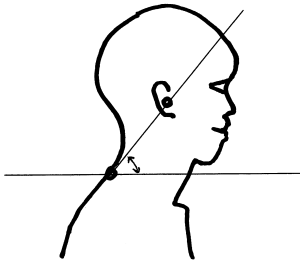
A typical chiropractic visit involves an assessment of posture and joint motion (possibly with the use of x-rays), helping the chiropractor assess the manner in which his/her patient exists and functions mechanically in a gravity environment. Abnormal findings are usually treated mechanically and primarily with the use of the chiropractic adjustment.
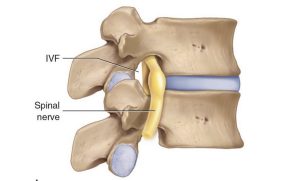
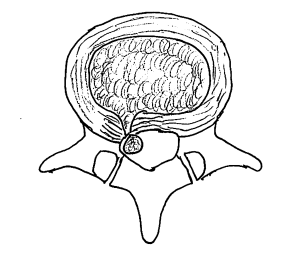
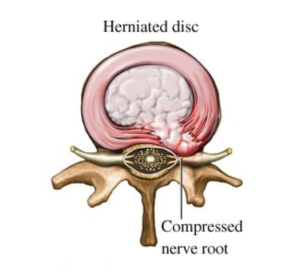
Early-on, many chiropractors were taught and believed that the physiological basis for their mechanical care was to treat compressive neuropathology (aka the “pinched nerve”). Although some chiropractic patients do suffer from compressive neuropathology, the majority (90+%) of their patients do not suffer from nerve compression (5).
It is now largely accepted that chiropractic adjustments mechanically activate a neurological sequence of events that close the pain gate (explained later) (5, 6, 7).
The primary points are that mechanical integrity in a gravity environment is important for how people feel and function, and that chiropractic adjusting influences mechanical integrity in a positive way. Chiropractors are trained to be mechanical providers of care. Ninety-three percent of patients who chose to initially see a chiropractor do so for spinal pain complaints (8). Satisfaction among patients with these complaints was exceptional (8).
The 2021 Nobel Prize in Physiology or Medicine
The 2021 Nobel Prize in Physiology or Medicine was awarded to David Julius, PhD, and Ardem Patapoutian, PhD (9, 10). Dr. Julius is a professor and chairman of the department of physiology at the University of California, San Francisco. Dr. Patapoutian is a professor at Scripps Research in La Jolla, California.
Their Nobel Prize included explaining the molecular basis for sensing mechanical forces, including how the body senses position and movement.
Understanding the importance of the neurological sensing of the mechanics of position and movement have been the core interest of the chiropractic profession since 1895. Despite many obstacles and often strong headwinds, the chiropractic profession has held steadfast to its mechanical/neurological roots. For more than a century, chiropractic clinicians and scientists have continued to explore and refine their mechanical applications of care, especially as related to musculoskeletal pain syndromes. The 2021 Noble Prize in Physiology or Medicine supports a century of data used by the chiropractic profession, which is briefly reviewed below.
•••
In 1921, Henry Winsor, MD, used 50 cadavers from the University of Pennsylvania and performed autopsies (necropsies) to determine whether there was any connection between spinal mechanical integrity and neurophysiological function (11). Dr. Winsor found, indeed, that spinal mechanical stiffness was common, advances with age, and is associated with deleterious neurological function.
•••
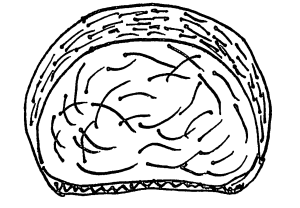
In the 1970s, Princeton University educated physiologist Irvin Korr, PhD, re-affirmed that spinal stiffness and/or aberrant motion altered the mechanical proprioceptive input into the central nervous system (12, 13). This aberrant neurological mechanical input would elicit abnormal spinal cord reflexes and abnormal signals to the brain, resulting in a variety of musculoskeletal dysfunctions.
•••
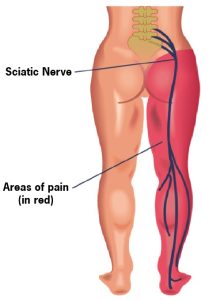
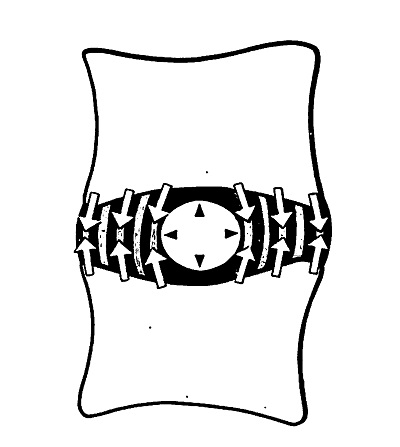
In 1985, William H. Kirkaldy-Willis, MD (Professor Emeritus of Orthopedics and director of the Low-Back Pain Clinic at University Hospital, Saskatoon, Canada), used the Gate Theory of Pain to explain the incredible reduction of back and leg pain in 283 subjects from chiropractic spinal adjusting (14).
The study was a prospective observational study. All 283 patients suffered from chronic low back and/or leg pain; they had also failed prior conservative and/or operative treatment, and they were all totally disabled. For those not suffering from compressive neuropathology, the clinical outcomes were outstanding in 81% of the subjects.
Dr. Kirkaldy-Willis noted that the Gate Theory of Pain has “withstood rigorous scientific scrutiny.” The Theory indicates that the central transmission of pain can be blocked by increased proprioceptive mechanical input. Spinal articular stiffness reduces proprioception (mechanoreception), “opening” the Pain Gate (increasing pain). Spinal adjusting improves articular motion, improves mechanoreception, and “closes” the Pain Gate (decreasing pain).
•••
In 1986 Vert Mooney, MD (orthopedic surgeon from the University of California, San Diego), was elected president of the International Society for the Study of the Lumbar Spine. His Presidential Address was published in the journal Spine the following year (15). In his Presidential Address to the Society, Dr. Mooney unfolds these concepts pertaining to the physiology of back pain:
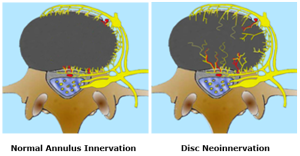
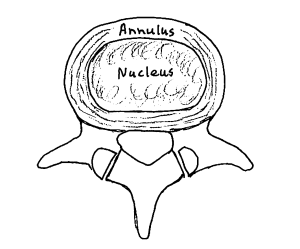
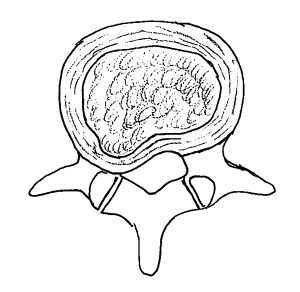
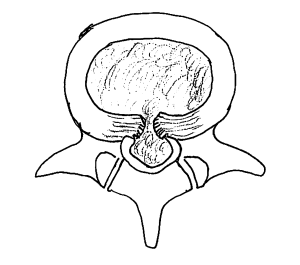
- Chronic low back pain primarily arises from the intervertebral disc.
- The intervertebral disc is avascular.
- An accumulation of inflammatory chemicals in the intervertebral disc initiates the nociceptive (pain) signal to the brain.
- The dispersion of the discogenic inflammatory nociceptive chemicals can only be achieved by improving the mechanical function of the intervertebral disc.
Key quotes from Dr. Mooney’s Presidential Address include:
“Mechanical events can be translated into chemical events related to pain.”
“Persistent pain in the back with referred pain to the leg is largely on the basis of abnormalities within the disc.”
“Mechanical activity has a great deal to do with the exchange of water and oxygen concentration [in the disc].”
“… research substantiates the view that unchanging posture, as a result of constant pressure such as standing, sitting or lying, leads to an interruption of pressure-dependent transfer of liquid. Actually, the human intervertebral disc lives because of movement.”
“In summary, what is the answer to the question of where is the pain coming from in the chronic low-back pain patient? I believe its source, ultimately, is in the disc. Basic studies and clinical experience suggest that mechanical therapy is the most rational approach to relief of this painful condition.”
•••
In 1992, Tuvia Mendel (Louisiana State University Medical Center) documented that the human cervical intervertebral disc is extensively innervated by mechanoreceptors, and that these mechanoreceptors are of considerable clinical importance in pain disorders of the spine (16). Mechanoreceptors were identified in every disc assessed.
Mr. Mendel notes that these mechanoreceptors provide basic proprioceptive function, specifically the sense of compression, deformation, and alignment. Key quotes from his study include:
“The presence of neural elements within the intervertebral disc indicates that the mechanical status of the disc is monitored by the central nervous system.”
“The location of the mechanoreceptors may enable the intervertebral disc to sense peripheral compression or deformation as well as alignment.”
•••
In 1994, Robert McLain, MD (then from the Department of Orthopedic Surgery, University of California, Davis, CA), documented that human cervical facet joints were innervated with mechanoreceptors (17). These mechanoreceptors provide basic proprioceptive function; they sense facet capsular tension, pressure, and position. Key quotes from his study include:
“Encapsulated mechanoreceptors are a consistent finding in normal human cervical facets.”
“The presence of these receptors in the facet capsule indicate that the mechanical state of the capsule (position, tension, pressure, etc.) is under the surveillance of the central nervous system.”
“The presence of mechanoreceptive and nociceptive nerve endings in cervical facet capsules proves that these tissues are monitored by the central nervous system and implies that neural input from the facets is important to proprioception and pain sensation in the cervical spine.”
•••
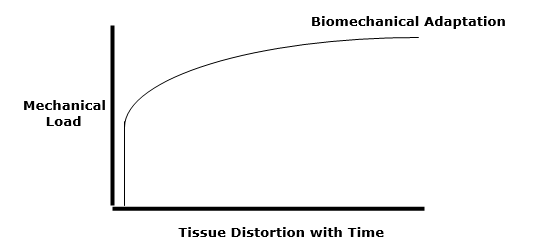
In 1998, Robert McLain, MD (then from the Department of Orthopedic Surgery, Cleveland Clinic, Ohio), published another study investigating the presence of mechanoreceptors in the facet joints of the thoracic and lumbar spines (18). Similar to his study on cervical spine mechanoreceptors, Dr. McLain established that the thoracic and lumbar facet joints are also innervated with mechanoreceptors. These mechanoreceptors provide basic proprioceptive function, including the sense of motion, tissue distortion, and position. Key quotes from his study include:
“Ongoing studies of spinal innervation have shown that human facet tissues contain mechanoreceptive endings capable of detecting motion and tissue distortion.”
“Encapsulated nerve endings are believed to be primarily mechanosensitive and may provide proprioceptive and protective information to the central nervous system regarding joint function and position.”
•••
In 1995, Sally Roberts, MD (RJAH Orthopaedic & District Hospital, Oswestry, Shropshire, UK), added to the evidence that human intervertebral discs are innervated with mechanoreceptors (19). She noted that these mechanoreceptors provide basic proprioceptive function, including the maintenance of muscle tone and muscular reflexes. Key quotes from her study include:
“[Physiologically, these mechanoreceptors] provide the individual with sensation of posture and movement.”
“In addition to providing proprioception, mechanoreceptors are thought to have roles in maintaining muscle tone and reflexes.”
“Their presence in the intervertebral disc and longitudinal ligament can have physiologic and clinical implications.”
•••
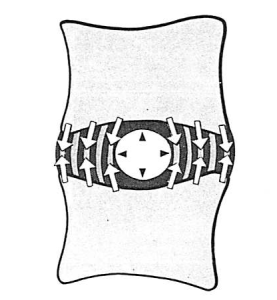
In his 2000 book titled Energy Medicine, James Oschman, PhD, describes a mechanically-based whole-body communication network that functions separately from the nervous system (20). In various parts of the book, Dr. Oschman terms this communication network “tensegrity,” or the “tensegrous matrix,” or the “tensegrous network.” Dr. Oschman amalgamates mechanical integrity and electromagnetic fields into human physiology.
Dr. Oschman’s book is fascinating and extremely important for providers of mechanically-based care and their patients. He includes a chapter pertaining to gravity and gravitational alignment, as well as a section on the value of chiropractic mechanically-based care. He also includes a section on the mechanics and the practice of orthopedics, as related to musculoskeletal pain syndromes.
•••
In 2003, Donald Ingber, MD, PhD (Vascular Biology Program, Departments of Surgery and Pathology, Children’s Hospital and Harvard Medical School), supported the writings of Dr. Oschman above by publishing a study on mechanotransduction and mechanobiology (21). Dr. Ingber notes that mechanical forces are critical regulators of cellular biochemistry and gene expression. He notes that mechanical forces are critical regulators in biology.
Dr. Ingber states that there is a strong mechanical basis for many generalized medical disabilities, such as lower back pain, which is responsible for a major share of healthcare costs world-wide. Physical interventions can influence cell and tissue function. This would include chiropractic care. Key quotes from his study include:
“Mechanical forces serve as important regulators at the cell and molecular levels, and they are equally potent as chemical cues.”
“In vitro and in vivo studies confirm that mechanical forces directly regulate the shape and function of essentially all cell types.”
•••
In 2006, Manohar Panjabi, PhD (Department of Orthopaedics and Rehabilitation, Yale University School of Medicine), proposed a new hypothesis to explain chronic back pain (22). He proposed that a single trauma or cumulative microtrauma can cause sub-failure injuries of the ligaments and their embedded mechanoreceptors. These injured mechanoreceptors generate corrupted signals leading to a poor muscle response pattern. This results in abnormal stresses and strains in the ligaments and joints, eventually producing chronic pain.
Dr. Panjabi emphasizes that the optimal approach to remedy this problem would target the function of the mechanoreceptors. Key quotes from his study include:
“Abnormal mechanics of the spinal column has been hypothesized to lead to back pain via nociceptive sensors.”
“Subfailure injuries of the ligaments and embedded mechanoreceptors generate corrupted mechanoreceptor signals.”
“The hypothesis proposes that the dysfunction of the muscle system over time may lead to chronic back pain via additional mechanoreceptor injury and neural tissue inflammation.”
•••
In 2010, Apostolos Dimitroulias, MD (Neurosurgical Department, Medical School, Aristotle University, Thessaloniki, Greece), evaluated the presence of mechanoreceptors in human lumbar (L4–5 and L5–S1) intervertebral discs (23).
Dr. Dimitroulias concluded that there is an abundant number of mechanoreceptors in the intervertebral discs of the lower lumbar spine in normal human subjects. The role of these mechanoreceptors is the continuous monitoring of position and movement. Abnormal mechanical information will produce muscle spasm, which is an important component of low back pain. A key quote from his study is:
“These receptors have a key role in the perception of joint position and adjustment of the muscle tone of the vertebral column.”
•••
Also, in 2010, James Wang, PhD, (Mechano-Biology Laboratory, Department of Orthopaedic Surgery, University of Pittsburgh School of Medicine) detailed how “Mechanics Rule Cell Biology.” (24) His study continues to support the studies by James Oshman and Donald Ingber above pertaining to the importance of tensegrity and mechanotransduction.
Dr. Wang notes that cellular mechanotransduction mechanisms convert mechanical force signals into biochemical signals in cells. He notes that “mechanics play a dominant role in cell biology.” He notes that the therapeutic use of mechanics is critical in improving health and function.
Key quotes from this study include:
“Mechanical forces are ubiquitous and are known to greatly influence physiology and pathophysiology in humans.”
“Mechanical forces have a profound effect on tissue homeostasis and pathophysiology.”
•••
In her 2017 book Move Your DNA: Restore Your Health Through Natural Movement, biomechanist Katy Bowman summarizes many of the mechanical concepts reviewed in this article (25). She integrates the importance of mechanoreceptors, gravity, alignment, posture, and motion, noting that “our bodies respond to mechanical input.” Key quotes from her book include:
“We should recognize our lack of health as a sign of a broken (mechanical) environment.”
“With respect to disease, the human’s internal mechanical environment has been the least-discussed environment of all—a staggering oversight when almost every cell in your body has specialized equipment just to sense the mechanical environment.”
“You can eat the perfect diet, sleep eight hours a night, and use only baking soda and vinegar to clean your house, but without the loads created by natural movement, all of these worthy efforts are thwarted on a cellular level, and your optimal wellness level remains elusive.”
“Human diseases are repeatedly explained to us in terms of their chemical or genetic makeup; meanwhile, we’ve completely ignored the load profile that the function of our body depends upon.”
“Whether out of convenience or ignorance, we have failed to address the habitat [‘habitual position relative to gravity’] in which our genes dwell, and the impact of the way we move on the state of our health.”
“Movement, position, and resting state of our musculoskeletal system are huge influencers of our mechanical environment.”
“Movement provides information for the body. Movement is an environmental or epigenetic factor. Our movement environment has been polluted.”
Katy Bowman’s book is incredibly consistent with the chiropractic perspective and chiropractic clinical practice.
•••
Summary
Mechanical providers of care have helped patients for millennia. Since 1895, in the United States and other countries around the world, the primary providers of mechanical care are chiropractors. The mechanical care delivered by chiropractors primarily influence special nerves that register the manner in which the individual is positioned and moves in a gravity environment. These specialized nerves are called mechanoreceptors. The studies reviewed here predict that the future of healthcare will involve mechanoreceptors and tensegrity. As noted, mechanoreceptors were awarded the Nobel Prize in Physiology or Medicine in October 2021. The status and future of chiropractic is looking very bright.
REFERENCES
- Morgan M; Mutant Message Down Under; 1990.
- Anderson R; “Spinal Manipulation Before Chiropractic”; in Haldeman S; Principles and Practice of Chiropractic; Second Edition; Appleton & Lang; 1992.
- Pettman E; A History of Manipulative Therapy; The Journal of Manual & Manipulative Therapy; 2007; Vol. 15; No. 3; pp. 165–174.
- cce-usa.org; accessed May 3, 2022.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Vicenzino B, Collins D, Wright A; The Initial Effects of a Cervical Spine Manipulative Physiotherapy Treatment on the Pain and Dysfunction of Lateral Epicondylalgia; Pain; November 1996; Vol. 68; No. 1; pp. 69-74.
- Savva C, Giakas G, Efstathiou M; The role of the descending inhibitory pain mechanism in musculoskeletal pain following high-velocity, low amplitude thrust manipulation: a review of the literature; Journal of Back and Musculoskeletal Rehabilitation; 2014; Vol. 27; No. 4; pp. 377-382.
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults: Results From the 2012 National Health Interview Survey; December 1, 2017; Spine; Vol. 42; No. 23; pp. 1810–1816.
- Roland D, Abott B; Nobel Prize in Medicine Awarded for Work on Senses; Wall Street Journal; October 5, 2021.
- Zylka MJ; A Nobel Prize for Sensational Research; New England Journal of Medicine; December 16, 2021; Vol. 385; No. 25; pp. 2393-2394.
- Winsor H; Sympathetic Segmental Disturbances: The Evidences of the Association, in Dissected Cadavers, of Visceral Disease with Vertebral Deformities of the Same Sympathetic Segments; Medical Times; November 1921; pp. 1-7.
- Korr IM; Proprioceptors and Somatic Dysfunction; Journal of the American Osteopathic Association; March 1975; Vol. 74; No. 7; pp. 638-650.
- Korr IM; The Spinal Cord as Organizer of Disease Process III: Hyperactivity of Sympathetic Innervation as a Common Factor in Disease; Journal of the American Osteopathic Association; December 1979; Vol. 79; No. 4; pp. 232-237.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Mooney V; Where Is the Pain Coming From?; Spine; October 1987; Vol. 12; No. 8; pp. 754-759.
- Mendel T, Wink CS, Zimny ML; Neural Elements in Human Cervical Intervertebral Discs; Spine; February 1992; Vol. 17; No. 2; pp. 132-135.
- McLain RF; Mechanoreceptor endings in human cervical facet joints; Spine; March 1, 1994; Vol. 19; No. 5; pp. 495-501.
- McLain RE, Pickar JG; Mechanoreceptor endings in human thoracic and lumbar facet joints; Spine; January 15, 1998; Vol. 23; No. 2; pp. 168-173.
- Roberts S, Eisenstein SM, Menage J, Evans EH, Ashton IK; Mechanoreceptors in intervertebral discs: Morphology, distribution, and neuropeptides; Spine; December 15, 1995; Vol. 20; No. 24; pp. 2645-2651.
- Oschman JL; Energy Medicine: The Scientific Basis; Churchill Livingstone; 2000.
- Ingber DE; Mechanobiology and Diseases of Mechanotransduction; Annals of Medicine; 2003; Vol. 35; No. 8; pp.564-577.
- Panjabi MM; A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction; European Spine Journal; May 2006; Vol. 15; No. 5; pp. 668-676.
- Dimitroulias A, Tsonidis C, Natsis K, Venizelos I, Djau SN. Tsitsopoulos P; An immunohistochemical study of mechanoreceptors in lumbar spine intervertebral discs; Journal of Clinical Neuroscience; June 2010; Vol. 17; No 6; pp. 742-745.
- Wang J, Bin Li; Mechanics Rule Cell Biology; Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology; 2010; Vol. 2; No. 16.
- Bowman K; Move Your DNA: Restore Your Health Through Natural Movement; 2017.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”