Chronic pain in the United States is an overwhelming, epidemic, problem. Of the 238 million adults in the US, 116 million suffer from chronic pain (1, 2). Quantifying the anatomical regions for American’s chronic pain shows that the fourth most common region of the body afflicted with chronic pain is the neck (3):
Hip Pain 07.1%
Finger Pain 07.6%
Shoulder Pain 09.0%
Neck Pain 15.1%
Severe Headache 16.1%
Knee Pain 19.5%
Lower-Back Pain 28.1%
Neck pain is a public health problem associated with disability, reduced health-related quality of life, and substantial health care system costs. A search of the National Library of Medicine of the United States (February 10, 2016) with PubMed, using the key words “neck pain manipulation” locates 759 articles.
••••••••••
In 2009, Mercer Health and Benefits released a study titled (4):
Do Chiropractic Services for the Treatment of Low Back and Neck Pain Improve the Value of Health Benefits Plans?
An Evidence-Based Assessment of Incremental Impact on Population Health and Total Health Care Spending
A Google Internet search of Mercer states:
“Mercer is a leading global provider of consulting, outsourcing and investment services. Mercer works with clients to solve their most complex benefit and human capital issues, designing and helping manage health, retirement and other benefits. It is a leader in benefit outsourcing. Mercer’s investment services include investment consulting and multi-manager investment management. Mercer’s 18,000 employees are based in more than 40 countries. The company is a wholly owned subsidiary of Marsh & McLennan Companies, Inc., which lists its stock on the New York, Chicago and London stock exchanges.”
Physicians Niteesh Choudhry, MD, PhD, and Arnold Milstein, MD, MPH, are the authors this Mercer report.
Dr. Niteesh Choudhry is from Harvard Medical School where he is an Assistant Professor of Medicine and an Associate Physician in the Division of Pharmaco-epidemiology and Pharmaco-economics. Dr. Arnold Milstein is from Mercer Health and Benefits in San Francisco, California where he is the Medical Director at Pacific Business Group on Health, the largest employer health care purchasing coalition in the US.
In this groundbreaking, authoritative document, Drs. Choudhry and Milstein note that neck pain is extremely common in the United States, and it consumes large amounts of health care resources. They note that about 14% of the US adult population report neck pain in a year. They make the following points:
“Low back and neck pain are extremely common conditions that consume large amounts of health care resources.”
“Chiropractic care, including spinal manipulation and mobilization, are used by almost half of the US patients with persistent back-pain seeking out this modality of treatment.”
“The peer-reviewed scientific literature evaluating the effectiveness of US chiropractic treatment for patients with back and neck pain suggest that these treatments are at least as effective as other widely used treatments.”
“Chiropractic care is more effective than other modalities for treating low back and neck pain.”
“Our findings in combination with existing US studies published in peer-reviewed scientific journals suggests that chiropractic care for the treatment of low back and neck pain is likely to achieve equal or better health outcomes at a cost that compares very favorably to most therapies that are routinely covered in US health benefit plans.”
“Using data from high-quality randomized controlled European trials and contemporary Unites States based average unit prices payable by commercial insurers, we project that insurance coverage for chiropractic coverage for chiropractic physician care for low back and neck pain for conditions other than fracture and malignancy is likely to drive improved cost-effectiveness of United States care.”
“For neck pain it is also likely to reduce total United States health care spending.”
“In combination with the existing United States-based literature, our findings support the value of health insurance coverage of chiropractic care for low back and neck pain at average fees currently payable by Unites States commercial insurers.”
This article by Mercer Health and Benefits is a unique analysis of the costs and effectiveness of chiropractic care in the management of low back and neck pain as compared to medical care and physiotherapy-led exercise. In the case of neck pain, chiropractic care was the most cost effective service, and its improvement in the quality-adjusted life year showed that if chiropractic care is used in the management of neck pain there would be a savings of $6,035 per person per year. Importantly, these authors indicate that chiropractic care is known to reduce the need for drug treatment.
••••••••••
In 2012, a study was published in the Annals of Internal Medicine, and titled (5):
Spinal Manipulation, Medication, or Home
Exercise With Advice for Acute and Subacute Neck Pain
A Randomized Trial
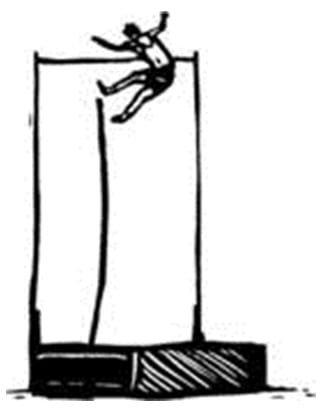
The authors note that mechanical neck pain is a common condition that affects an estimated 70% of persons at some point in their lives. This study sought to determine the relative efficacy of chiropractic spinal manipulation therapy (SMT), medication, and home exercise with advice (HEA) for acute and subacute neck pain in both the short and long term. This is a randomized, controlled trial using 272 subjects aged 18 to 65 years who had nonspecific neck pain for 2 to 12 weeks. The intervention was 12 weeks of SMT, medication, or HEA.
The chiropractic spinal manipulation focused on manipulation of areas of the spine with segmental hypomobility. The primary measurement outcome was participant-rated pain, measured at 2, 4, 8, 12, 26, and 52 weeks after randomization. Secondary measures were self-reported disability, global improvement, medication use, satisfaction, general health status (Short Form-36 Health Survey physical and mental health scales), and adverse events.
Results: For neck pain, chiropractic spinal manipulation had a statistically significant advantage over medication after 8, 12, 26, and 52 weeks, and HEA was superior to medication at 26 weeks. The authors concluded that for participants with acute and subacute neck pain, chiropractic spinal manipulation was more effective than medication in both the short and long term.
The home exercise with advice was provided in two 1-hour sessions. The therapists provided instruction, primarily focusing on simple self-mobilization exercise (gentle controlled movement) of the neck and shoulder joints, including neck retraction, extension, flexion, rotation, lateral bending motions, and scapular retraction, with no resistance. Participants were instructed to do 5 to 10 repetitions of each exercise up to 6 to 8 times per day. A booklet (McKenzie R. Treat Your Own Neck. 3rd ed. Waikanae, New Zealand: Spinal Publications; 2002) of prescribed exercises was provided.
The medication group was provided by a licensed medical physician, with the focus of treatment on prescription medication. The first line of therapy was nonsteroidal anti-inflammatory drugs, acetaminophen, or both.
Participants who did not respond to or could not tolerate first-line therapy received narcotic medications. Muscle relaxants were also used.
The authors made these comments:
“Spinal manipulation therapy was superior to medication at the end of treatment and during follow-up in terms of global improvement, participant satisfaction, and SF-36 –assessed physical function; SMT was also superior to medication in measures of long-term medication use.”
“The SMT and HEA groups performed similarly on most of the secondary outcomes, although SMT performed better than HEA for satisfaction with care in both the short and long term.”
“Spinal manipulation therapy and HEA led to similar short- and long-term outcomes, but participants who received medication seemed to fare worse, with a consistently higher use of pain medication for neck pain throughout the trial’s observation period.”
“Our results suggest that SMT and HEA both constitute viable treatment options for managing acute and subacute mechanical neck pain.”
Thus, the mechanical approaches to acute/subacute neck pain management were shown not only to be significantly more effective than medication, but also significantly safer.
Although the printed words in the article suggest that chiropractic spinal adjusting and home exercise/advice are essentially equal in the management of acute and subacute neck pain, a careful review of the measured markers presented in the article show that chiropractic adjustments were nearly always superior to those from home exercise/advice.
Although the article states several times that the chiropractic adjustments were given over a period of 12 weeks, the actual range of adjustments was 2-23 with a mean of 15.3. This is slightly more than 1 adjustment per week for 12 weeks. In contrast, the home exercise/advice group was seen only 1 or 2 times, but instructed to do neck exercises at home daily. The exercises consisted of 7 isolated maneuvers that required 3 different positions: sitting, supine head supported, and supine head unsupported. Each maneuver required 10 repetitions, and the patient was instructed to repeat all of the maneuvers 6-8 times per day. Performing the exercise maneuvers as prescribed takes approximately 10 minutes per session. As such, the authors are advocating that patients with acute/subacute neck pain exercise 60-80 minutes per day; this is both impractical and unrealistic.
Considering these issues, chiropractic spinal manipulation was more effective and much more practical than pharmacology and home exercise advise in the treatment of these neck pain subjects.
••••••••••
Another study from 2012 was published in the Journal of Orthopaedic & Sports Physical Therapy, and titled (6):
Upper Cervical and Upper Thoracic Thrust Manipulation Versus Nonthrust Mobilization in Patients With Mechanical Neck Pain:
A Multicenter Randomized Clinical Trial
The authors note that a bout 54% of individuals have experienced neck pain within the last 6 months. The economic burden associated with the management of patients with neck pain is high, second only to low back pain in annual workers’ compensation costs in the United States.
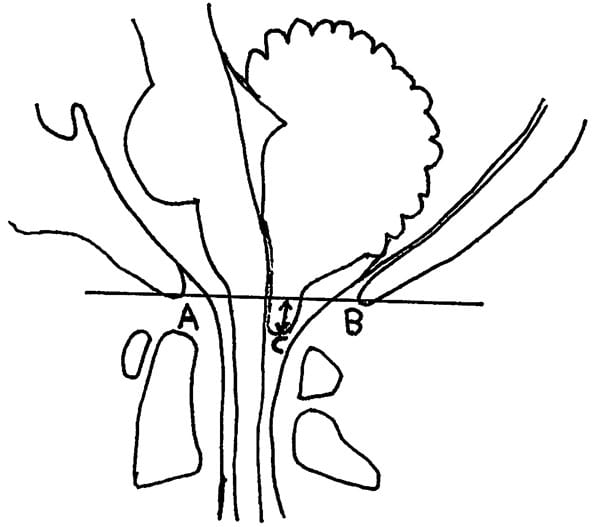
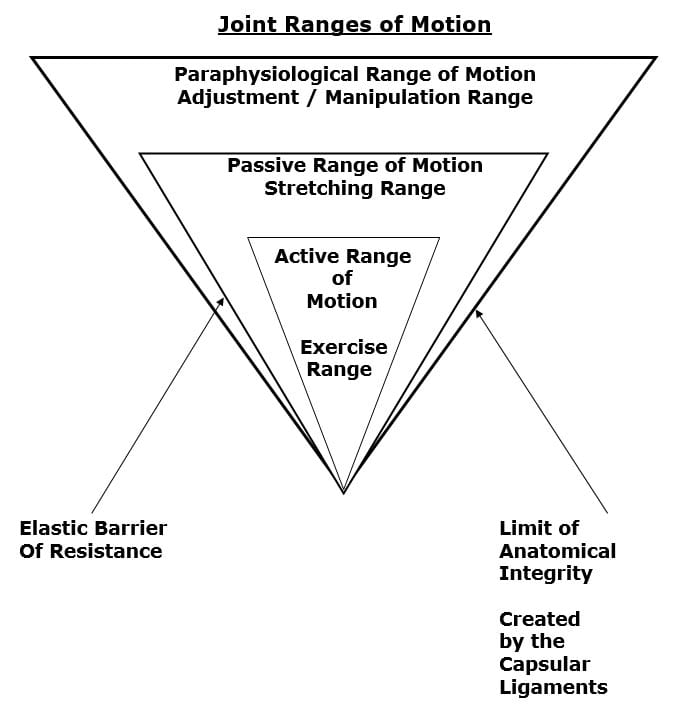
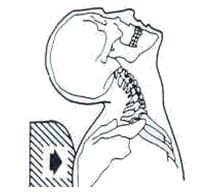
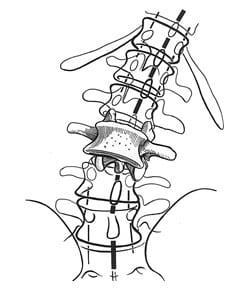
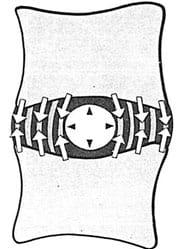
This study is a randomized clinical trial to compare the short-term effects of upper cervical and upper thoracic high-velocity low-amplitude (HVLA) thrust manipulation to nonthrust mobilization in patients with neck pain. Although upper cervical and upper thoracic HVLA thrust manipulation and nonthrust mobilization are common interventions for the management of neck pain, no studies have directly compared the effects of both upper cervical and upper thoracic HVLA thrust manipulation to nonthrust mobilization in patients with neck pain.
In this study, 107 neck pain participants were evaluated subjectively and objectively, and then randomized to receive either HVLA thrust manipulation or nonthrust mobilization to the upper cervical (C1-2) and upper thoracic (T1-2) spines (n = 56) or nonthrust mobilization (n = 51).
The participants were reexamined 48-hours after the initial examination/treatment and again completed the outcome measures. The effects of treatment on disability, pain, C1-2 passive rotation range of motion, and motor performance of the deep cervical flexors were examined.
The patients with mechanical neck pain who received the combination of upper cervical and upper thoracic HVLA thrust manipulation experienced significantly greater reductions in disability (50.5%) and pain (58.5%) than those of the nonthrust mobilization group (12.8% and 12.6%, respectively) following treatment. In addition, the HVLA thrust manipulation group had significantly greater improvement in both passive C1-2 rotation range of motion and motor performance of the deep cervical flexor muscles as compared to the group that received nonthrust mobilization.
The authors concluded that the combination of upper cervical and upper thoracic HVLA thrust manipulation is appreciably more effective in the short term than nonthrust mobilization in patients with mechanical neck pain.
The C1-2 articulation has a high frequency of involvement in patients with neck pain and headaches. Disturbances in joint mobility in the upper thoracic spine may be an underlying contributor to musculoskeletal disorders in the cervical spine. Decreased mobility in the cervicothoracic junction (C7-T2) is associated with mechanical neck pain.
The primary outcome measure used in this study was the patient’s perceived level of disability as measured by the Neck Disability Index (NDI). The NDI is the most widely used condition-specific disability scale for patients with neck pain. The NDI has been demonstrated to be a reliable and valid outcome measure for patients with neck pain.
The authors state:
“A single session of HVLA thrust manipulation directed to both the upper cervical and upper thoracic spines results in greater improvements in disability, pain, atlantoaxial joint ROM, and motor performance of the deep cervical flexor muscles than nonthrust mobilization directed to the same regions.”
“We directed treatment to the atlantoaxial joints, because the C1-2 articulation has been found to have a high frequency of symptomatic involvement in patients with neck pain and headaches and previous studies have demonstrated that this articulation is where the majority of cervical rotation occurs.”
“The results of the current study demonstrated that patients with mechanical neck pain who received the combination of upper cervical and upper thoracic HVLA thrust manipulation, experienced greater reduction in pain and disability, showed greater improvement in passive C1-2 rotation range of motion, and had greater increases in motor performance of the deep cervical flexor muscles, as compared to the group that received nonthrust mobilization at a 48-hour follow-up visit.”
“The combination of HVLA thrust manipulation procedures directed to both the upper cervical and upper thoracic articulations may enhance the overall outcomes of patients with mechanical neck pain.”
Nonthrust mobilization is not worthless; it clearly helped the patients in this study. However, thrust/cavitation manipulations of the same spinal regions (upper cervical and upper thoracic spines) were significantly superior to mobilization in:
1) Overall successful outcomes
2) Disability reduction
3) Pain reduction
4) Increased cervical range of motion
5) Improvements in motor performance of the deep cervical flexors
Also, this study indicates that upper cervical and upper thoracic spines are biomechanically functionally linked and that the superior results achieved in this study as compared to other studies is as a consequence of adjusting both regions.
••••••••••
In September 2015, researchers and clinicians from the Orthopedic University Hospital Balgrist, University of Zurich, Switzerland, published a study in the Journal of Manipulative and Physiological Therapeutics, titled (7):
Prognostic Factors for Recurrences in Neck Pain Patients Up to 1 Year After Chiropractic Care
This is a prospective cohort study assessing 545 neck pain patients. After a course of chiropractic spinal manipulation, they were followed up for one year regarding recurrence of their neck pain. Nine independent prognostic variables were assessed:
• Age
• Use of pain medication
• Sex
• Work status
• Duration of complaint
• Previous episodes of neck pain
• Trauma onset
• Numeric Rating Scale (NRS) was used to quantify their pain
• Bournemouth Questionnaire was used for neck pain
These authors note that most people will see a health care provider at least once in their lifetime due to neck pain. In patient populations that do not include chiropractic care, those who have experienced an episode of neck pain are likely to have another episode within the next 1 to 5 years. Overall, for these individuals, the prognosis for a complete recovery from their neck pain is “quite poor.” Those who do not recover from their neck pain within the 3 months after treatment begins tend to suffer from residual neck pain and disability.
There are known prognostic factors for the onset of neck pain. They include:
• Computer work
• Heavy physical work
• Longer duration of complaint
• Older age
• Female sex
• Previous neck injury
The results of this study are impressive:
• Fifty-four (54) participants (11%) were identified as “recurrent.”
• Four hundred ninety one (491) participants (89%) were not recurrent.
The authors state:
“89% of neck pain patients had recovered from their neck pain episode up to 1 year after receiving chiropractic care.”
This study also found that older age and a previous episode of neck pain were useful predictors of neck pain recurrence within 1 year. This is because an increase in age was associated with recurrence. Patients older than 45 years are twice as likely to experience a neck pain recurrence within 1 year after the start of chiropractic treatment. They state:
“Having had a previous episode as well as increasing age are increased risk factors for predicting a subsequent new episode of neck pain within a year.”
These authors concluded:
“The results of this study suggest that recurrence of neck pain within 1 year after chiropractic intervention is low.”
This study indicates that chiropractic is both effective in the treatment of neck pain and that its benefits are stable and long lasting.
••••••••••
The years 2000-2010 were designated as The Bone and Joint Decade. In 2008, the Bone and Joint Decade Task Force on Neck Pain and its Associated Disorders (Neck Pain Task Force) published its initial assessment pertaining to neck pain in the journal Spine (8, 9). An international team of experts did the assessment. The study design was to establish “Best Evidence Synthesis.” The researchers identified, critically appraised, and synthesized literature from 1980 through 2006 on noninvasive interventions for neck pain and its associated disorders. The researchers identified 359 articles deemed to be relevant, and 170 (47%) were accepted as scientifically admissible. The group’s conclusion was (9):
“Our best evidence synthesis suggests that therapies involving manual therapy and exercise are more effective than alternative strategies for patients with neck pain.”
The manual therapy references included both mobilization and manipulation. Thus, as of a review of the best literature up through 2006 (and published in 2008), mobilization and manipulation were included in the best evidence for the noninvasive treatment of neck pain.
In 2015, a second international group of experts once again reviewed the literature to further refine the “best evidence” for the treatment of neck pain (10). The authors were from:
- Canadian Memorial Chiropractic College
- University of Ontario
- Mount Sinai Hospital
- University of Toronto
- University of Alberta
- University of Montreal
- Queen’s University
- New York University
The purpose of this study was to update the findings of the Neck Pain Task Force (from 2008) by continuing to examine the effectiveness of manual therapies, passive physical modalities, and acupuncture for the management of whiplash associated disorders or neck associated disorders. The authors performed a systematic review and best evidence synthesis including randomized controlled trials, cohort studies, and case-control studies comparing manual therapies, passive physical modalities, or acupuncture to other interventions, placebo/sham, or no intervention. They searched five databases from 2000 to 2014, screening 8,551 citations, finding 38 studies to be most relevant. The authors state:
“We also found that there were no serious adverse events reported in randomized clinical trials on manipulation.”
“Our review adds new evidence to the Neck Pain Task Force and suggests that mobilization, manipulation, and clinical massage are effective interventions for the management of neck pain.”
“Our update of the Neck Pain Task Force suggests that mobilization, manipulation, and clinical massage are effective interventions for the management of neck pain.”
These authors note there is difficulty in comparing different types of studies for many different reasons. Despite such difficulties, they still conclude that manual therapy, both mobilization and manipulation are effective in the treatment of whiplash-associated disorders and other neck pain syndromes, and that both are quite safe (“there were no serious adverse events reported in randomized clinical trials on manipulation.”) In short, the best evidence available, early published in December 2015, concludes that spinal manipulation and manipulation are both safe and effective in the treatment of patients with neck pain.
SUMMARY
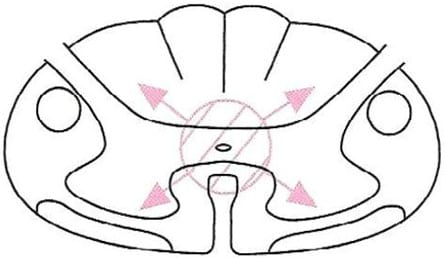
Both acute and chronic neck pain is primarily attributed to the facet joints. This is especially true of those injured in a whiplash-mechanism accident. Chiropractic spinal adjusting (specific joint manipulation) affects many tissues, but primarily the facet joints. Evidence continues to support that spinal manipulation is both effective and safe for patients suffering with neck pain, including patients with neck pain initiated by a whiplash injury. The evidence supports spinal manipulation for both acute and chronic neck pain/. The evidence also shows that spinal manipulation is not only effective, but the benefits are also long-lasting with only a small incidence of recurrence.
REFERENCES
- Foreman J; A Nation in Pain, Healing Our Biggest Health Problem; Oxford University Press; 2014.
- Pho, K; USA TODAY, The Forum; September 19, 2011; pg. 9A.
- Wang S; Why Does Chronic Pain Hurt Some People More?; Wall Street Journal; October 7, 2013.
- Choudhry N, Milstein A; Do Chiropractic Services for the Treatment of Low Back and Neck Pain Improve the Value of Health Benefits Plans? An Evidence-Based Assessment of Incremental Impact on Population Health and Total Health Care Spending; Mercer Health and Benefits; 2009.
- Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, MS; Grimm RH; Spinal Manipulation, Medication, or Home Exercise With Advice for Acute and Subacute Neck Pain: A Randomized Trial; Annals of Internal Medicine; January 3, 2012; Vol. 156; pp. 1-10.
- Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, Sigurdsson G; Upper Cervical and Upper Thoracic Thrust Manipulation Versus Nonthrust Mobilization in Patients With Mechanical Neck Pain: A Multicenter Randomized Clinical Trial; Journal of Orthopaedic & Sports Physical Therapy; January 2012; Volume 42; Number 1; pp. 5-18.
- Langenfeld A, Humphreys K, Swanenburg J, Cynthia K. Peterson CK; Prognostic Factors for Recurrences in Neck Pain Patients Up to 1 Year After Chiropractic Care; Journal of Manipulative and Physiological Therapeutics; September 2015; Vol. 38; No. 7; pp. 458-464.
- Guzman J, Haldeman S, Carroll LJ, et al. Clinical practice implications of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. Spine (Phila Pa 1976) 2008;33:S199-213.
- Hurwitz EL, Carragee EJ, van der Velde G, et al; Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33:S123-52.
- Jessica J. Wong, Heather M. Shearer, Silvano Mior, Craig Jacobs, Pierre Côté, Kristi Randhawa, Hainan Yu, Danielle Southerst, Sharanya Varatharajan, Deborah Sutton, Gabrielle van der Velde, Linda J. Carroll, Arthur Ameis, Carlo Ammendolia, Robert Brison, Margareta Nordin, Maja Stupar, Anne Taylor-Vaisey; Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders?; An update of the Bone and Joint Decade Task Force on Neck Pain and its Associated Disorders by the OPTIMa Collaboration; The Spine Journal; December 2015 [epub]
- Bogduk N, Aprill C; On the nature of neck pain, discography and cervical zygapophysial joint blocks; Pain; August 1993; Vol. 54; No. 2; pp. 213-217.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”