In biomechanics, there is a rule that notes that the regions of the body that have the greatest mobility have the least stability; and reduced stability is coupled with greater injury and stress risk. Joints that have multiple planes of motion are particularly prone to increased stress and injury risk.
The jaw not only open and closes, it can move side-to-side as well as protrude forward and retract backwards. These diverse planes of motion increase the risk for biomechanical problems.
The jaw is used in talking, chewing, swallowing, kissing, yawning, and in facial expressions. It is vulnerable to injury during trauma such as whiplash exposure, boxing, and other impact/collision-types of sports or activities. Certain types of psychometric stress can cause night grinding, stressing the jaw joint.
The jawbone is attached to the skull. Anatomically, the jawbone is known as the mandible. The skull is comprised of many different bones that are tightly bound together. The skull bone where the mandible attaches is anatomically known as the temporal bone. The joint between the mandible and the temporal bone is the temporomandibular joint, commonly abbreviated TMJ.
Disorders of the temporomandibular joint (TMJ), are referred to as the temporomandibular dysfunction, commonly abbreviated TMD.
Dental and facial experts have long understood that the function of the TMJ is inherently linked to the biomechanical function of the neck (the cervical spine). This is because of shared neurology.
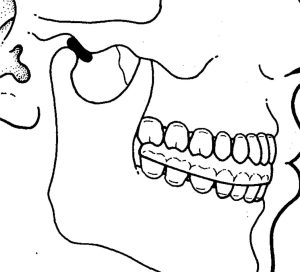
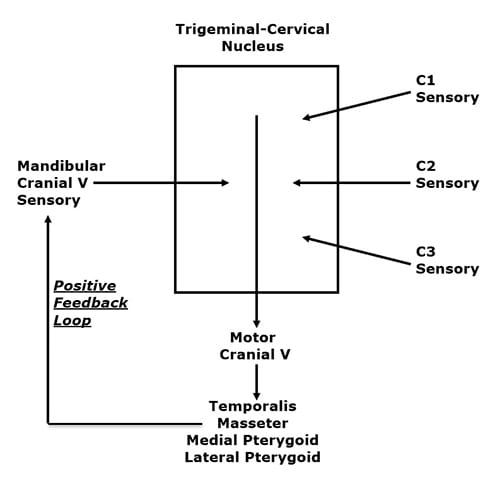
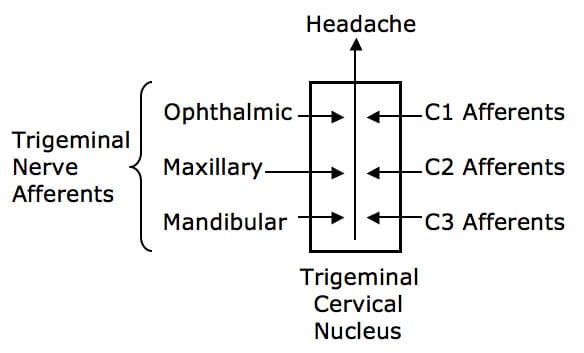
The TMJ, like all other moveable joints, has two primary categories of nerves: sensory and motor. The sensory nerves provide to the brain information such as pain, temperature, and position. The motor nerves move the joint by directing the contraction of the muscles that cross the TMJ. The motor and sensory nerves to the TMJ largely travel and exist together in the mandibular branch of the trigeminal nerve (cranial nerve V).
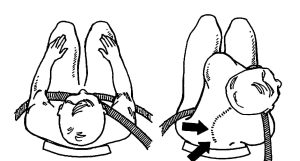
There are four muscles that cross the TMJ and control the movement of this joint. They are (also noted in the drawing above):
- Temporalis
- Masseter
- Medial Pterygoid
- Lateral Pterygoid
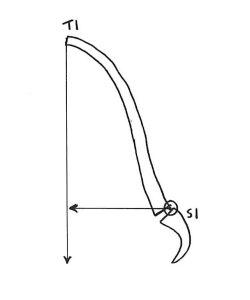
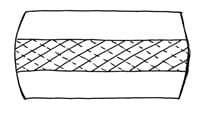
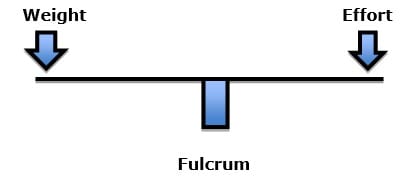
Please look at the drawing above. In a unique anatomical occurrence, the sensory nerve (mandibular cranial V) that innervates the TMJ, the motor nerves that move the TMJ, and the sensory nerves of the upper neck (cervicals 1-2-3), all communicate with each other in a “box,” depicted above, called the trigeminocervical nucleus. Functionally, this means that neck problems that involve the upper cervical spine nerve roots (C1, C2, C3) have the ability to influence the motor nerves that control the muscles that cross the TMJ. Again, upper neck problems can activate the four muscles that move the TMJ (temporalis, masseter, medial and lateral pterygoid muscles).
A muscular imbalance of the TMJ can cause TMJ biomechanical stress and inflammation. The consequence of this is depolarization of the sensory nerves that innervate the TMJ, causing pain and other symptoms (discussed below). This TMJ sensory disturbance sends afferent information into the trigeminocervical nucleus, creating a positive feedback loop (see above drawing), ultimately resulting in temporomandibular dysfunction (TMD).
The pertinent question for this review is:
Can biomechanical treatment, specifically chiropractic spinal manipulation, of the upper cervical spine that reduces aberrant sensory input from the upper cervical spinal nerves, be successful in the management of TMD?
•••••
A noted authoritative reference text pertaining to the jaw is the 1991 book titled (1):
Temporomandibular Disorders, Diagnosis and Treatment
The lead author is Andrew Kaplan, DMD. Dr. Kaplan’s credentials include:
- Director, Temporomandibular Disorder/Facial Pain Clinic, The Mount Sinai Hospital
- Assistant Clinical Professor, The Mount Sinai Hospital
- Coordinator, Department of Dentistry, The Mount Sinai Hospital
- Clinical Instructor, Department of Medicine, Hospital Division, New York University
Co-author Leon Assael, DMD, has an equally impressive resume:
- Associate Professor and Residency Program Director, Department of Oral and Maxillofacial Surgery, University of Connecticut School of Dental Medicine
- Associate Professor of Surgery, School of Medicine, University of Connecticut
- Associate Chief of Staff, John Dempsey Hospital
- Attending Oral and Maxillofacial Surgeon, Hartford Hospital, Hartford, Connecticut
Their book has 31 distinguished contributing authors, 35 chapters, and 754 pages.
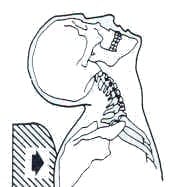
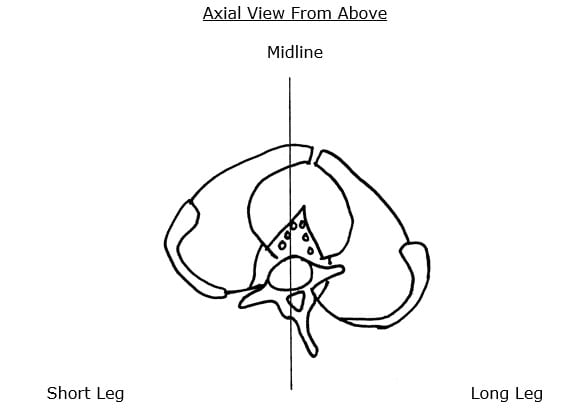
Drs. Kaplan and Assael’s text discusses scenarios where altered neuro-biomechanical function of the cervical spine can put stress on the TMJ causing TMD. They note that temporomandibular joint pain may occur as a consequence of forward head posture.
The most common TMD symptom is pain just in front of the tragus of the ear. Other common symptoms include clicking, crepitation, transient locking, locking with restricted mandibular movements, and mandibular deflection. TMD is also related to headache, dizziness, earache, and auditory disturbances.
It is increasingly being accepted that disorders of the cervical spine can cause temporomandibular disorders, even in the absence of direct injury or stress to the temporomandibular joint. In such cases, although the symptoms may be attributed to the jaw, the treatment is to the cervical spine.
•••••
In 1998, the journal Clinical Oral Investigations, published a study titled (2):
Correlation Between Cervical Spine
and Temporomandibular Disorders
The authors evaluated 31 consecutive patients with symptoms of temporomandibular disorders and 30 controls with a standardized clinical examination of the masticatory system, evaluating range of motion of the mandible, temporomandibular joint function and pain of the temporomandibular joints and masticatory muscles. Afterwards subjects were referred for clinical examination of the cervical spine, evaluating segmental limitations, tender points upon palpation of the muscles, hyperalgesia, and hypermobility.
The results indicated that segmental limitations, especially at the occiput-C3 levels, and tender points, especially in the sternocleidomastoid and trapezius muscles, were significantly more present in patients than in controls.
The authors concluded that the “temporomandibular system and the cervical spine function as a single entity.”
•••••
In 2004 the European Journal of Oral Sciences published a study titled (3):
Deranged Jaw–Neck Motor Control
in Whiplash-Associated Disorders
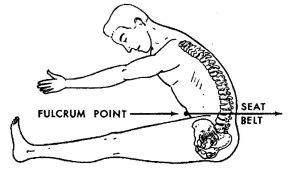
The authors noted that jaw movements are the result of activation of the jaw as well as the neck muscles, leading to simultaneous movements in the temporomandibular, atlanto-occipital and cervical spine joints. Therefore, injury to the neck would disturb natural jaw function. Anatomical, biomechanical, neuroanatomical, neurophysiological and clinical studies indicate that the mandibular and the craniocervical regions are functionally linked. Natural jaw activities require a healthy state of both the mandibular and the head–neck motor systems. Natural jaw actions require a healthy state not only of the temporomandibular joint but also of the atlanto-occipital and cervical spine joints. Neck trauma can be an etiological factor behind temporomandibular disorders. Neck injury from whiplash is associated with deranged control of mandibular movements which compromise jaw function.
The authors present evidence that supports that whiplash injuries to the cervical spine alter the normal function of the TMJ. Injury to the upper cervical spine causes a reflex to the TMJ muscles, causing TMD.
•••••
In 2008, the Swedish Dental Journal published a study titled (4):
Impaired Jaw Function and Eating Difficulties
in Whiplash-Associated Disorders
These authors evaluated 50 whiplash-injured patients with pain and dysfunction in the jaw-face region and 50 healthy age- and sex-matched controls without any history of neck injury. For the whiplash-injured group, there were significantly differences in jaw pain, jaw dysfunction, and eating behavior after the accident. The whiplash-injured patients after the accident reported pain and dysfunction during mouth opening, biting, chewing, swallowing, and yawning and felt fatigue, stiffness, and numbness in the jaw-face region. A majority also reported avoiding tough food and big pieces of food, and taking breaks during meals.
These authors noted that jaw opening-closing movements are the result of coordinated activation of both jaw and neck muscles, with simultaneous movements in the temporomandibular, atlanto-occipital and cervical spine joints. Consequently, pain or dysfunction in any of the three joint systems involved could impair jaw activities.
•••••
In 2015, CRANIO, The Journal of Craniomandibular & Sleep Practice, published a study titled (5):
Upper Cervical Range of Motion is Impaired
in Patients with Temporomandibular Disorders
The authors note that clinicians are increasingly suggesting assessment and treatment of the cervical spine in patients with temporomandibular dysfunction (TMD). The purpose of this study was to investigate whether patients with TMD pain present with upper cervical spine impairment when compared with asymptomatic subjects.
The authors evaluated 37 subjects with TMD and compared them to 20 asymptomatic control subjects by comparing cervical range of motion (ROM) measures.
The authors found significant differences in upper the cervical spine range of motion between the TMD group and the control group. They concluded:
“This study provides evidence for the importance of examination of upper cervical mobility in patients who suffer from TMD.”
•••••
In 2016, the journal Manual Therapy published a study titled (6):
Do Subjects with Acute/Subacute Temporomandibular Disorder
Have Associated Cervical Impairments: A Cross-Sectional Study
The authors note that there is evidence of cervical musculoskeletal impairment in some temporomandibular disorder (TMD) pain states. Therefore they conducted a cross-sectional survey to determine whether people with TMD have more cervical signs of dysfunction than healthy subjects. Ninety-nine TMD subjects were evaluated for signs of cervical musculoskeletal impairment and disability as compared to a control group of 45 subjects.
The authors found that the control group without TMD was consistently less impaired in cervical spine function. The authors note:
“The more dysfunction and pain is identified in the temporomandibular region, the greater levels of dysfunction is observable on a number of cervical musculoskeletal function tests.”
“These findings provide evidence that TMD is strongly related with certain cervical spine musculoskeletal impairments which suggests the cervical spine should be examined in patients with TMD as a potential contributing factor.”
•••••
A recent study was published in June 2018 in the journal Manuelle Medizin [The European Journal of Manual Medicine], titled (7):
Spinal High-Velocity Low-Amplitude Manipulation with Exercise
in Women with Chronic Temporomandibular Disorders:
A Randomized Controlled Trial Comparing to Patient Education
This study is the first prospective randomized controlled clinical trial to directly compare the effectiveness of upper cervical manipulation, sham manipulation, and education in patients with temporomandibular disorders.
The objective of this study was to investigate the effects of spinal high-velocity low-amplitude manipulation with exercise compared to patient education in patients with chronic temporomandibular disorders (TMD). Fifty-five female patients (age 18-50 years) with temporomandibular disorders were randomized to three groups:
- Cervical spinal manipulation plus neck exercise (CSM + NE)
- Sham manipulation plus neck exercise (SM + NE)
- Patient education only (PE)
Patient assessments were done at baseline, post-treatment (a minimum of 6 treatment sessions), and at a 1-month follow-up. Assessments were performed using:
- Numeric rating scale / NRS for pain intensity
- Pressure pain thresholds / PPT masseter/temporalis muscles
- Pain-free maximum mouth opening / MMO in millimeters
- Short Form 36 / SF-36 for quality of life
The cervical manipulations were applied to the upper cervical spine. The authors state:
“Cervical spinal manipulation was performed using a segment-specific technique for segmental dysfunctions of the upper cervical spine.”
The manipulation applied in this study appeared to be a sitting rotational maneuver. The physician’s middle finger was placed on the C1 transverse process. The manipulation was done posterior to anterior. Slack taken up to “exclude contraindications (such as pain or dizziness during the test) against an impulse.”
The sham spine manipulation was performed using a high-velocity low-amplitude manipulation to “give the patient the same mechanical and acoustic sensations.” It was applied to the cervico-thoracic junction by an “impulse to the spinous process of C7.”
The authors note that “temporomandibular disorders are musculoskeletal conditions characterized by painful conditions and dysfunctions in the muscles of mastication, the temporomandibular joint, and related-tissue components.”
The prevalence of temporomandibular disorders is between 3% and 15% of the population. They primarily affect middle-aged adults. Women are affected twice as often as men.
Classic TMD disorders symptoms are headache and neck pain. The authors note that because of the “neuroanatomical convergence of trigeminal and upper cervical afferents in the medullary dorsal horn of the spinal cord (trigeminal caudal nucleus),” that:
“Cervical dysfunctions can influence the temporomandibular system.”
The authors found:
“Significant differences were observed in the cervical spinal manipulation plus neck exercise group vs. the sham manipulation plus neck exercise and patient education only groups post-treatment.”
There was “significantly increased [in pressure pain thresholds] in the upper cervical manipulation group, while there were no changes in the pressure pain thresholds in both the sham manipulation and education groups.”
There were significant increases of pain-free maximum mouth opening post-treatment in the cervical spinal manipulation groups.
There were significant increases in the Short Form-36 scores post-treatment in the cervical spinal manipulation group.
There was significant improvement in the Numeric Rating Scale in the cervical spinal manipulation group.
The authors concluded:
“It is highly likely that functional integration exists between jaw and cervical movements.”
“This prospective randomized controlled trial demonstrates that in the presence of temporomandibular disorders, the high-velocity low-amplitude manipulation of the upper cervical spine combined with a neck exercise program reduced jaw pain intensity and increased the pressure pain thresholds of masseter and temporalis muscles as well as pain-free maximum mouth opening; moreover, it improved quality of life in women with temporomandibular disorders after treatment and at the 1-month follow up.”
“Our study suggests that high-velocity low-amplitude manipulation of the upper cervical spine with neck exercise can be effective for treatment of pain and dysfunction in patients with chronic temporomandibular disorders.”
“It seems reasonable to add cervical manipulation to the rehabilitation program.”
“Cervical manipulation might positively influence cervical movements, which can affect temporomandibular movements if cervical dysfunction is present.”
“Our data provide new evidence about the efficacy of treatment for temporomandibular disorders focused on the upper cervical region.”
“High-velocity low-amplitude manipulation andneck exercise was used for the management of patients with chronic temporomandibular disorders.”
“Our study proves that upper cervical spine manipulations play an important role in the treatment of pain and dysfunction in the presence of temporomandibular disorders by interruption of the nociceptive vice versa effects of trigemino-cervical convergence.”
•••••
SUMMARY
TMD problems and symptoms are common within the population. It is often assumed that TMD problems are attributed to dysfunctions of the TMJ. This review notes that there is an intimate neurological functional relationship between the TMJ and the upper cervical spine. It is proposed that the best management of TMD involves both evaluation and treatment of the upper cervical spine, and that optimal treatment involves upper cervical spinal manipulation.
In patients with upper neck, jaw, face or head pain, both the cervical spine and temporomandibular joints should be evaluated. This review implies that perhaps an explanation for chronic TMD is failure to evaluate and treat the upper cervical spine.
REFERENCES:
- Kaplan A, Assael L; Temporomandibular Disorders, Diagnosis and Treatment; WB Saunders Company; 1991.
- De Laat A, Meuleman H, Stevens A, Verbeke G; Correlation Between Cervical Spine and Temporomandibular Disorders; Clinical Oral Investigations; June 1998; Vol. 2; No. 2; pp. 54-57.
- Eriksson PO, Zafar H, Haggman-Henrikson B; Deranged jaw–neck motor control in whiplash-associated disorders; European Journal of Oral Sciences; February, 2004; Vol. 112; pp. 25–32.
- Grönqvist J, Häggman-Henrikson B, Eriksson PO; Impaired jaw function and eating difficulties in whiplash-associated disorders; Swedish Dental Journal; 2008; Vol. 32; No. 4; pp.171-177.
- Grondin F, Hall T, Laurentjoye M, Ella B; Upper cervical range of motion is impaired in patients with temporomandibular disorders; CRANIO, The Journal of Craniomandibular & Sleep Practice; April 2015 Vol. 33; No. 2; pp. 91-99.
- von Piekartz H, Pudelko A, Danzeisen M, Hall T, Ballenberger N; Do subjects with acute/subacute temporomandibular disorder have associated cervical impairments: A cross-sectional study; Manual Therapy; December 2016; Vol. 26; pp. 208-215.
- Corum M, Basoglu C, Topaloglu M, Dıracoglu D; Aksoy C; Spinal High-Velocity Low-Amplitude Manipulation with Exercise in Women with Chronic Temporomandibular Disorders: A Randomized Controlled Trial Comparing to Patient Education; Manuelle Medizin [The European Journal of Manual Medicine]; June 2018; Vol. 56; No. 3; pp. 230–238.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”