Spinal Manipulation for Lumbar Intervertebral Disc Syndrome with Radiculopathy
For thirty years (since 1985), it has been acknowledged that spinal manipulation is successful in the treatment of the majority of patients with low back pain, and that “there is a scientific basis for the treatment of back pain by manipulation.” (1) However, the consensus pertaining to the use of spinal manipulation for the treatment of intervertebral disc syndrome with radiculopathy is less investigated. Consequently, there is the potential for an opinion that spinal manipulation may be inappropriate for patients with low back intervertebral disc syndrome and symptoms/signs of radiculopathy. This publication will review a number of articles on this topic, spanning six decades (1954-2015).
••••••••••
In 1954, RH Ramsey, MD, published a study titled (2):
Conservative Treatment of Intervertebral Disk Lesions
Dr. Ramsey’s study appeared in the Instructional Course Lectures of the American Academy of Orthopedic Surgeons. Dr. Ramsey states:
“The conservative management of lumbar disk lesions should be given careful consideration because no patient should be considered for surgical treatment without first having failed to respond to an adequate program of conservative treatment.”
“If after a fair trial of conservative treatment, the pain and disability continue and the symptoms are of sufficient gravity to warrant surgery, the patient is advised that he should be operated upon and the offending disk lesion should be removed.”
Dr. Ramsey advocated a number of conservative treatments for this syndrome, including spinal manipulation. Pertaining to manipulation, Dr. Ramsey makes the following comments:
“From what is known about the pathology of lumbar disk lesions, it would seem that the ideal form of conservative treatment would theoretically be a manipulative closed reduction of the displaced disk material.”
“Many forms of manipulation are carried out by orthopaedic surgeons and by cultists and this form of treatment will probably always be a controversial one.”
“We limit the use of manipulation almost entirely to those patients who do not seem to be responding well to non-manipulative conservative treatment and who are anxious to have something else done short of operative intervention.”
“The patient lies on his side on the edge of the table facing the surgeon and the leg that is up is allowed to drop over the side of the table, tending to swing the up-side of the pelvis forward. The arm that is up is allowed to drop back behind the patient, tending to pull the shoulder back. The surgeon then places one hand on the patient’s shoulder and his opposite forearm on the patient’s iliac crest. Simultaneously, the shoulder is thrust suddenly back, rotating the torso in one direction while the iliac crest is thrust down and forward, rotating the pelvis in the opposite direction. This gives the lumbar spine a twist that frequently causes an audible and palpable crunch. This procedure is then repeated with the patient on his other side. The patient is then turned on his back and his hips and knees are hyperflexed sufficiently to forcibly flex the lumbar spine which tends to open up the disk spaces posteriorly.”
“The patient should be cautioned beforehand that forceful manipulation may possibly make his symptoms worse although many patients will get marked relief.”
Dr. Ramsey notes that the manipulation is “forceful” and associated with an “audible and palpable crunch.” Although he cautions that the manipulation may make the patient worse, “many patients will get marked relief.”
••••••••••
Fifteen years later (in 1969), physicians JA Mathews and DAH Yates from the Department of Physical Medicine, St. Thomas’ Hospital, London, published a study titled (3):
Reduction of Lumbar Disc Prolapse by Manipulation
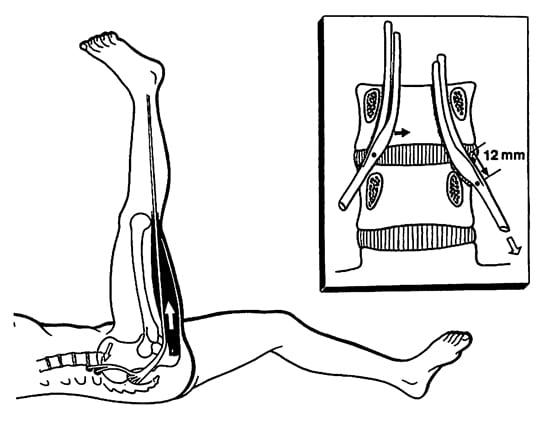
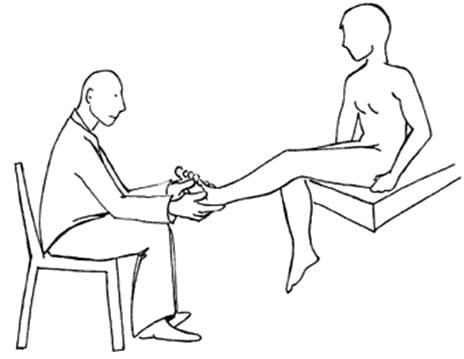
This study appeared in the September 20, 1969 issue of the British Medical Journal. These authors evaluated a number of patients that presented with an acute onset of low back and buttock pain that did not respond to rest. Diagnostic epidurography showed a clinically relevant small disc protrusion, along with antalgia and positive lumbar spine nerve stretch tests. These patients were then treated with long-lever rotation manipulations of the lumbar spine, using the shoulder and iliac crest as levers. These lumbar spine manipulations were clearly accompanied with a thrust maneuver. The manipulations were repeated until abnormal symptoms and signs had disappeared. Following the manipulations there was resolution of signs, symptoms, antalgia, and reduction in the size of the protrusions. Drs. Mathews and Yates state:
“The frequent accompaniment of acute onset low back pain by spinal deformity suggests a mechanical factor, and the accompanying abnormality of straight-leg raise or femoral stretch test suggests that the lesion impinges on the spinal dura matter of the dural nerve sheaths.”
“The lumbar spine was rotated away from the painful side to the limit of its range, the buttock or thigh of the painful side being used as a lever; a firm additional thrust was made in the same direction. This manoeuver was repeated until abnormal symptoms and signs had disappeared, progress being assessed by repeated examination.”
“Rotation manipulations apply torsion stress throughout the lumbar spine. If the posterior longitudinal ligament and the annulus fibrosus are intact, some of this torsion force would tend to exert a centripetal force, reducing prolapsed or bulging disc material.”
“The results of this study suggest that small disc protrusions were present in patients presenting with lumbago and that the protrusions were diminished in size when their symptoms had been relieved by manipulations.”
These authors conclude: “it seems likely that the reduction effect [of the disc protrusion] is due to the manipulating thrust used.”
••••••••••
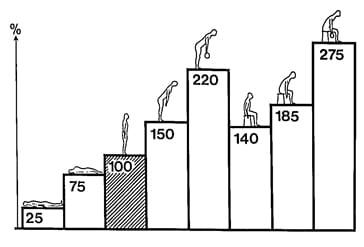
In another study published in 1969, BC Edwards compared the effectiveness of heat/massage/exercise to spinal manipulation in the treatment of 184 patients that were grouped according to the presentation of back and leg pain, as follows (4):
|
Group |
Treatment |
Acceptable Outcome |
|
Central Low Back Pain Only |
heat/massage/exercise |
83% |
|
spinal manipulation |
83% |
|
|
Pain Radiation to Buttock |
heat/massage/exercise |
70% |
|
spinal manipulation |
78% |
|
|
Pain Radiation Down Thigh to Knee |
heat/massage/exercise |
65% |
|
spinal manipulation |
96% |
|
|
Pain Radiation down Leg to Foot |
heat/massage/exercise |
52% |
|
spinal manipulation |
79% |
This study by Edwards was published in the Australian Journal of Physiotherapy.
This study by Edwards was reviewed by Augustus A. White, MD, and Manohar M. Panjabi, PhD, in their 1990 book, Clinical Biomechanics of the Spine (5). Drs. White and Panjabi make the following points pertaining to the Edwards article:
“A well-designed, well executed, and well-analyzed study.”
In the group with central low back pain only, “the results were acceptable in 83% for both treatments. However, they were achieved with spinal manipulation using about one-half the number of treatments that were needed for heat, massage, and exercise.”
In the group with pain radiating into the buttock, “the results were slightly better with manipulation, and again they were achieved with about half as many treatments.”
In the groups with pain radiation to the knee and/or to the foot, “the manipulation therapy was statistically significantly better,” and in the group with pain radiating to the foot, “the manipulative therapy is significantly better.”
“This study certainly supports the efficacy of spinal manipulative therapy in comparison with heat, massage, and exercise. The results (80 – 95% satisfactory) are impressive in comparison with any form of therapy.”
••••••••••
In 1977, the third edition of Orthopaedics, Principles and Their Applications was published. The author, Samuel Turek, MD (d. 1986), was a Clinical Professor, Department of Orthopedics and Rehabilitation at the University of Miami School of Medicine. In the section pertaining to the protruded disc, Dr. Turek makes the following observations (6):
Treatment of Intervertebral Disc Herniation With Manipulation
“Manipulation. Some orthopaedic surgeons practice manipulation in an effort at repositioning the disc. This treatment is regarded as controversial and a form of quackery by many men. However, the author has attempted the maneuver in patients who did not respond to bed rest and were regarded as candidates for surgery. Occasionally, the results were dramatic.
Technique. The patient lies on his side on the edge of the table facing the surgeon, and the uppermost leg is allowed to drop forward over the edge of the table, carrying forward that side of the pelvis. The uppermost arm is placed backward behind the patient, pulling the shoulder back. The surgeon places one hand on the shoulder and the other on the iliac crest and twists the torso by pushing the shoulder backward and the iliac crest forward. The maneuver is sudden and forceful and frequently is associated with an audible and palpable crunching sound in the lower back. When this is felt, the relief of pain is usually immediate. The maneuver is repeated with the patient on the opposite side.”
“The patient should be cautioned beforehand that the manipulation may make his symptoms worse and that this is an attempt to avoid surgery.”
••••••••••
In February 1987, physicians Paul Pang-Fu Kuo and Zhen-Chao Loh published an important study pertaining to lumbar disc protrusions and rotary spinal manipulation, titled (7):
Treatment of Lumbar Intervertebral Disc Protrusions by Manipulation
Their article appeared in the journal Clinical Orthopedics and Related Research. Drs. Paul Pang-Fu Kuo and Zhen-Chao Loh are from the Department of Orthopedic Surgery, Shanghai Second Medical College, and Chief Surgeon, Department of Orthopaedic Surgery, Rui Jin Hospital, Shanghai, China. They note that manipulation has been used in Chinese healthcare for thousands of years, and by the Tang Dynasty (618-907 AD), who noted “manipulation was fully established and became a routine for the treatment of low back pain.”
In their study, they performed a series of eight manipulations on 517 patients with protruded lumbar discs and clinically relevant signs and symptoms. Their outcomes were quite good, with 84% achieving a successful outcome and only 9% not responding. Only 14 % suffered a reoccurrence of symptoms at intervals ranging from two months to twelve years. These authors state:
“The patient is placed on the sound side first with the hip and knee of the painful side flexed and the sound side straight. The operator rests one hand in front of the shoulder and the other hand on the buttock. By simultaneously pulling the shoulder backwards and pushing the buttock forwards, a snap or click can usually be heard or felt. This manipulation may then be repeated on the other side as required.”
“Manipulation of the spine can be effective treatment for lumbar disc protrusions.”
“Most protruded discs may be manipulated. When the diagnosis is in doubt, gentle force should be used at first as a trial in order to gain the confidence of the patient.”
“During manipulation a snap may accompany rotation. Subjectively it has dramatic influence on both patient and operator and is thought to be a sign of relief.”
“If derangement of the facets or subluxation of the posterior elements near the protruded disc occurs, the rotation may have caused reduction, giving remarkable relief.”
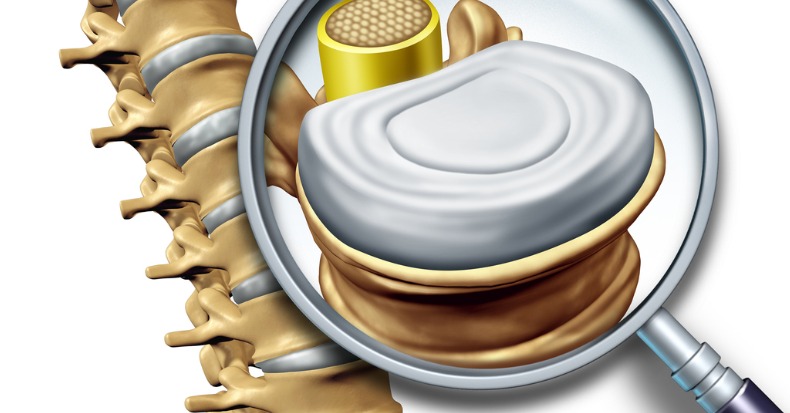
“Gapping of the disc on bending and rotation may create a condition favorable for the possible reentry of the protruded disc into the intervertebral cavity, or the rotary manipulation may cause the protruded disc to shift away from pressing on the nerve root.”
In terms of applying manipulation, Drs. Kuo and Loh indicate “practice is necessary to become proficient in spinal manipulation techniques,” and “expertise plays an important role in the success of manipulation.” The manipulation of disc protrusions should be performed only by trained experts. Additionally, manipulation is contraindicated if the patient is suffering from incontinence or paraplegia.
••••••••••
In 1989, the Journal of Manipulative and Physiological Therapeutics published a case study of a patient with an “enormous central herniation lumbar disc” who underwent a course of side posture manipulation (8). The patient improved considerably with only 2 weeks of treatment. The authors state:
“It is emphasized that manipulation has been shown to be an effective treatment for some patients with lumbar disc herniation.
While complications of this form of treatment have been reported in the literature, such incidents are rare.”
••••••••••
In 1993, chiropractor J. David Cassidy, chiropractor Haymo Thiel, and physician (orthopedic surgeon) William Kirkaldy-Willis published a “Review Of The Literature” article titled (9):
Side posture manipulation for lumbar intervertebral disk herniation
These authors are from the Department of Orthopaedics, Royal University Hospital, Saskatoon, Saskatchewan, Canada, and their article appeared in the Journal of Manipulative and Physiological Therapeutics.
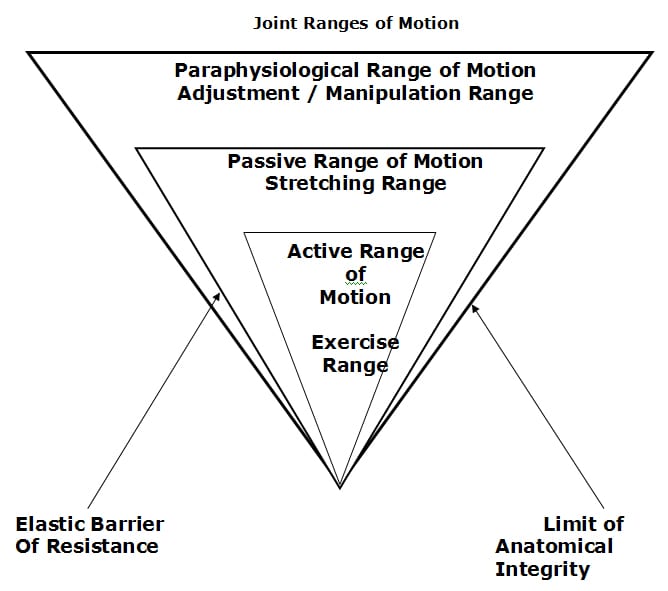
In their article, these authors cite studies on human cadavers that show the annulus of the disc is quite resistant to rotational stresses. Specifically, a normal disc did not show failure until 22.6° of rotational stress, and a degenerated disc could withstand an average of 14.3° of rotational stress. They therefore conclude “torsional failure of the lumbar disk first requires fracture of the posterior joints” before there is any annular tearing.
When performing rotational manipulation in the management of lumbar disc herniation, these authors suggest that it is wise to begin with mobilization prior to performing manipulation to assess the patients responses. Additionally, they state that if positioning increases leg pain, “one should not proceed to manipulation at that particular session.”
Based upon their review of the literature and their own experiences, these authors state:
“The treatment of lumbar disk herniation by side posture manipulation is not new and has been advocated by both chiropractors and medical manipulators.”
“The treatment of lumbar intervertebral disk herniation by side posture manipulation is both safe and effective.”
••••••••••
In 1995, chiropractors PJ Stern, Peter Côté P, and David Cassidy published a study titled (10):
A series of consecutive cases of low back pain with radiating leg pain treated by chiropractors
Their article appeared in the Journal of Manipulative and Physiological Therapeutics. The authors retrospectively reviewed the outcomes of 59 consecutive patients complaining of low back and radiating leg pain, and were clinically diagnosed as having a lumbar spine disk herniation. Ninety percent of these patients reported improvement of their complaint after chiropractic manipulation. The maximum complication rate associated with this treatment approach was estimated to be 5% or less. A previous history of low back surgery was a statistically significant predictor of poor outcome. They concluded:
“Based on our results, we postulate that a course of non- operative treatment including manipulation may be effective and safe for the treatment of back and radiating leg pain.”
••••••••••
In 2006, physicians Valter Santilli, MD, Ettore Beghi, MD, Stefano Finucci, MD, published an article in The Spine Journal titled (11):
Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion:
A randomized double-blind clinical trial of active and simulated spinal manipulations
The purpose of this study was to assess the short- and long-term effects of spinal manipulations on acute back pain and sciatica with disc protrusion. It is a randomized double-blind trial comparing active and simulated manipulations for these patients. The study used 102 patients. The manipulations or simulated manipulations were done 5 days per week by experienced chiropractors for up to a maximum of 20 patient visits, “using a rapid thrust technique.” Re-evaluations were done at 15, 30, 45, 90, and 180 days.
The authors list rationales for using manipulation in the treatment of low back pain and sciatica to include:
- Reduction of a bulging disc
- Correction of disc displacement
- Release of adhesive fibrosis surrounding prolapsed discs or facet joints
- Release of entrapped synovial folds
- Inhibition of nociceptive impulses
- Relaxation of hypertonic muscles
- Unbuckling displaced motion segments
The authors noted the following observations:
“Active manipulations have more effect than simulated manipulations on pain relief for acute back pain and sciatica with disc protrusion.”
“At the end of follow-up a significant difference was present between active and simulated manipulations in the percentage of cases becoming pain-free (local pain 28% vs. 6%; radiating pain 55% vs. 20%).”
“Patients receiving active manipulations enjoyed significantly greater relief of local and radiating acute LBP, spent fewer days with moderate-to-severe pain, and consumed fewer drugs for the control of pain.”
“No adverse events were reported.”
The authors concluded that chiropractic spinal “manipulations may relieve acute back pain and sciatica with disc protrusion.”
|
Real Manipulations |
Simulated Manipulations |
|
|
# of Subjects |
53 |
49 |
|
% of Local Pain Free Subjects |
28% |
6% |
|
% of Radiation Pain Free Subjects |
55% |
20% |
••••••••••
In 2014, an interdisciplinary group of physicians, chiropractors, and researchers published a study in the Annals of Internal Medicine, titled (12):
Spinal Manipulation and Home Exercise With Advice for Subacute and Chronic Back-Related Leg Pain
This study was funded by the United States Department of Health and Human Services. It included 192 patients who were suffering from back-related leg pain for least 4 weeks. The number of subjects in the study gave it good statistical power. The subjects were randomized into either:
- Chiropractic spinal manipulation + home exercise and advice, or
- Home exercise and advice alone
The treatment lasted 12 weeks. The authors concluded:
“For leg pain, spinal manipulative therapy plus home exercise and advice had a clinically important advantage over home exercise and advice (difference, 10 percentage points) at 12 weeks.”
“Spinal manipulative therapy with home exercise and advice improved self-reported pain and function outcomes more than exercise and advice alone at 12 weeks.”
“Spinal manipulative therapy combined with home exercise and advice can improve short-term outcomes in patients with back-related leg pain.”
“For patients with subacute and chronic back-related leg pain, spinal manipulative therapy in addition to home exercise and advice is a safe and effective conservative treatment approach, resulting in better short-term outcomes than home exercise and advice alone.”
“No serious treatment-related adverse events or deaths occurred.”
••••••••••
In another 2014 study, a group of multidisciplinary researchers and chiropractic clinicians from Switzerland presented a prospective study involving 148 patients with low back and leg pain. The study was published in the Journal of Manipulative and Physiological Therapeutics and titled (13):
Outcomes of Acute and Chronic Patients with Magnetic Resonance Imaging–Confirmed Symptomatic Lumbar Disc Herniations Receiving High-Velocity, Low-Amplitude, Spinal Manipulative Therapy:
A Prospective Observational Cohort Study With One-Year Follow-Up
The purpose of this study was to document outcomes of patients with confirmed, symptomatic lumbar disc herniations and sciatica that were treated with chiropractic side posture high-velocity, low-amplitude, spinal manipulation to the level of the disc herniation. It is important to emphasize that all patients in this study had clear abnormal physical examination findings of radiculopathy, including positive MRI abnormalities that corresponded with their symptoms and physical findings. Their pain was rated using the numerical rating scale and their disability was measured with the Oswestry questionnaire. Evaluations were performed at 2 weeks, 1 month, 3 months, 6 months, and 12 months.
The outcomes from this study are summarized in the following table:
Substantial Improvement (rounded)
|
|
2 weeks |
1 month |
3 months |
6 months |
12 months |
|
Entire group |
70% |
80% |
91% |
89% |
88% |
|
Acute group |
81% |
85% |
95% |
91% |
86% |
|
Chronic group |
47% |
71% |
82% |
89% |
89% |
The authors make the following statements:
“The proportion of patients reporting clinically relevant improvement in this current study is surprisingly good, with nearly 70% of patients improved as early as 2 weeks after the start of treatment. By 3 months, this figure was up to 90.5% and then stabilized at 6 months and 1 year.”
“A large percentage of acute and importantly chronic lumbar disc herniation patients treated with chiropractic spinal manipulation reported clinically relevant improvement.”
“Even the chronic patients in this study, with the mean duration of their symptoms being over 450 days, reported significant improvement, although this takes slightly longer.”
“A large percentage of acute and importantly chronic lumbar disc herniation patients treated with high-velocity, low- amplitude side posture spinal manipulative therapy reported clinically relevant ‘improvement’ with no serious adverse events.”
“Spinal Manipulative therapy is a very safe and cost-effective option for treating symptomatic lumbar disc herniation.”
This study shows that patients with proven lumbar intervertebral disc herniation and compressive neuropathology that receive traditional chiropractic side-posture manipulation is both safe and effective. The ultimate clinical effectiveness of about 90% is impressive when compared to any form of therapy, and with no reported serious side effects.
This study would suggest that all patients suffering from lumbar intervertebral disc herniation with compressive neuropathology should be treated with chiropractic spinal adjusting.
- Kirkaldy-Willis WH, Cassidy, JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985, Vol. 31, pp. 535-540.
- Ramsey RH; Conservative Treatment of Intervertebral Disk Lesions; American Academy of Orthopedic Surgeons, Instructional Course Lectures; Volume 11, 1954, pp. 118-120.
- Mathews JA and Yates DAH; Reduction of Lumbar Disc Prolapse by Manipulation; British Medical Journal; September 20, 1969, No. 3, 696-697.
- Edwards BC; Low back pain and pain resulting from lumbar spine conditions: a comparison of treatment results; Australian Journal of Physiotherapy; 15:104, 1969.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second edition, JB Lippincott Company, 1990.
- Turek S; Orthopaedics, Principles and Their Applications; JB Lippincott Company; 1977; page 1335.
- Kuo PP and Loh ZC; Treatment of Lumbar Intervertebral Disc Protrusions by Manipulation; Clinical Orthopedics and Related Research. No. 215, February 1987, pp. 47-55.
- Quon JA, Cassidy JD, O’Connor SM, Kirkaldy-Willis WH; Lumbar intervertebral disc herniation: treatment by rotational manipulation; Journal of Manipulative and Physiological Therapeutics; 1989 Jun;12(3):220-7.
- Cassidy JD, Thiel HW, Kirkaldy-Willis WH; Side posture manipulation for lumbar intervertebral disk herniation; Journal of Manipulative and Physiological Therapeutics; February 1993;16(2):96-103.
- Stern PJ, Côté P, Cassidy JD; A series of consecutive cases of low back pain with radiating leg pain treated by chiropractors; Journal of Manipulative and Physiological Therapeutics; 1995 Jul-Aug;18(6):335-42.
- Santilli V, Beghi E, Finucci S; Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: A randomized double-blind clinical trial of active and simulated spinal manipulations; The Spine Journal; March-April 2006; Vol. 6; No. 2; pp. 131–137.
- Bronfort G, Hondras M, Schulz CA, Evans RL, Long CR, PhD; Grimm R; Spinal Manipulation and Home Exercise With Advice for Subacute and Chronic Back-Related Leg Pain; A Trial With Adaptive Allocation; Annals of Internal Medicine; September 16, 2014; Vol. 161; No. 6; pp. 381-391.
- Leemann S, Peterson CK, Schmid C, Anklin B, Humphreys BK; Outcomes of Acute and Chronic Patients with Magnetic Resonance Imaging–Confirmed Symptomatic Lumbar Disc Herniations Receiving High-Velocity, Low Amplitude, Spinal Manipulative Therapy: A Prospective Observational Cohort Study With One-Year Follow-Up; Journal of Manipulative and Physiological Therapeutics; March/April 2014; Vol. 37; No. 3; pp. 155-163.