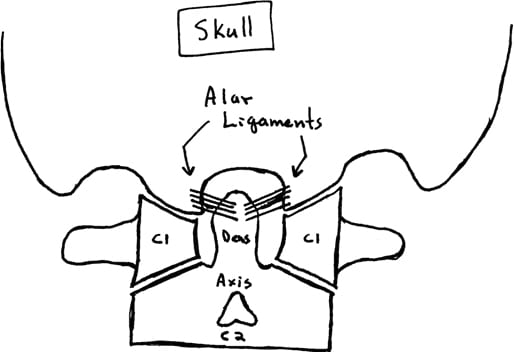
The understanding of whiplash biomechanics was forever changed in 1997. Researchers from Yale University School of Medicine performed a series of rear-end collisions on human cadavers while imaging their biomechanics with cineradiography (1). The results established that during the earliest phase of collision mechanics, the cervical spine forms an “S” shaped configuration, with flexion of the upper cervical spine and simultaneous significant hyperextension of the lower cervical spine. The tissue distortion noted during this “S” configuration of the cervical spine was of a magnitude that is injurious, especially in the lower cervical spine. As the subjects used in this initial assessment were cadavers, skepticism as to the relevance to live humans in real life collisions remained. This skepticism was mitigated within a few years with follow-up studies.
In 1999, similar cineradiography studies were performed on live human volunteers (2). The results were the same as those of the cadaver studies, solidifying the concept that the cervical spine undergoes an “S” configuration during a rear-end motor vehicle collision, primarily injuring structures of the lower cervical spine. Essentially all articles published between 1997–1999 regarding whiplash biomechanics cite these studies, noting that the pathology of whiplash primarily occurs during this “S” configuration. A representative article from 2007 states (3):
“The forward acceleration of the torso deforms the cervical spine into a non-physiologic S-shaped curve, with extension developing between the lower segments and flexion developing between the uppermost segments. Most of the whiplash injury occurs during this deformation phase.”
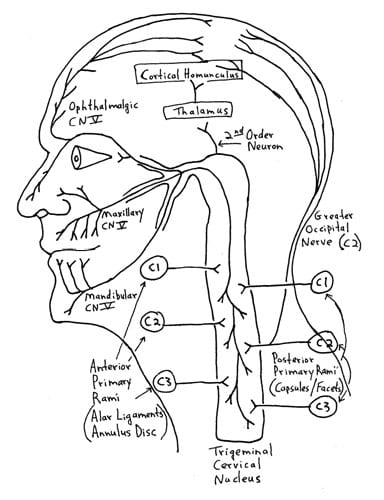
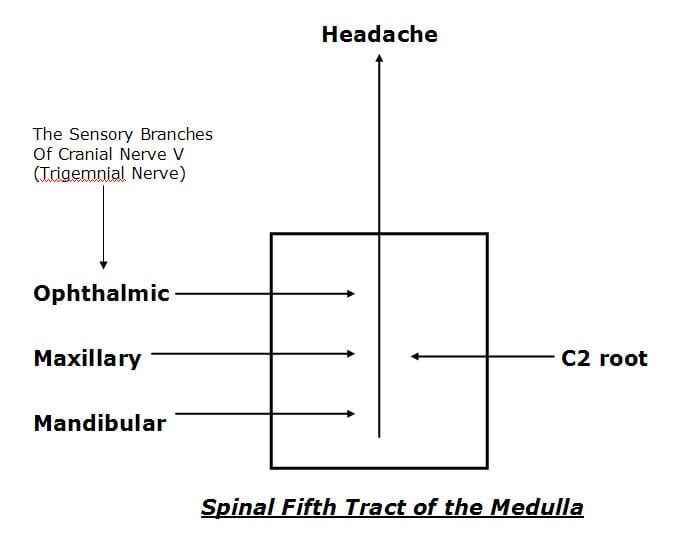
“The cervical facet joint is the most common source of chronic neck pain after whiplash injury.”
“The facet joints are the most common source of chronic neck pain after whiplash injury.”
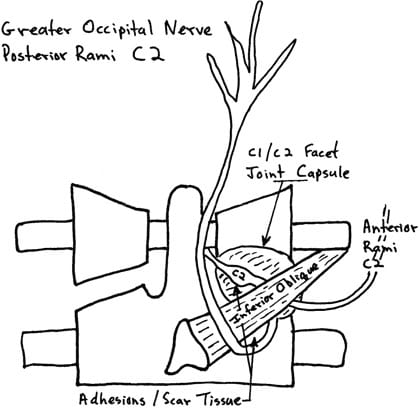
Injury to the facet joints and their capsular ligaments as a consequence of the “S” configuration should be emphasized. Findings include (2):
“The zygapophysial joint is the suspected origin of neck pain after rear-end car collision.”
“Most whiplash injuries occur during low-speed rear-end collisions and rarely produce morphologic changes such as fracture of the joint. The zygapophysial joint is a synovial joint and has a synovial fold (meniscus), between the articular facets that is innervated with nociceptive receptors. Thus, we hypothesize that facet collisions are likely to impinge on and inflame the synovial folds in the zygapophysial joints, causing neck pain (facet synovial fold impingement syndrome).”
Many other studies support the premise of whiplash-mechanism facet joint injury and pain (4, 5, 6, 7, 8, 9, 10).
•••••••••
The entire December 1, 2011 supplement of the journal Spine is dedicated to whiplash trauma. The issue contains 27 articles by the world’s foremost authorities on whiplash biomechanics, pathology and outcomes, including the physician/clinical anatomist, Nikoli Bogduk, from Australia. Dr. Bogduk’s article in this issue of Spine is titled, “On Cervical Zygapophysial Joint Pain After Whiplash” (9).
Dr. Bogduk cites 72 references while summarizing the evidence that implicates the cervical zygapophysial joints (facets) as the leading source of chronic neck pain after whiplash trauma. He states that the patho-anatomic basis for neck pain after whiplash is not elusive, but rather well documented and well known. Dr. Bogduk notes that there is convergent validity from
- whiplash postmortem studies
- whiplash biomechanics studies
- whiplash clinical studies
All of these studies and diverse methods of investigation indicate that the primary source of chronic whiplash pain is injury to the cervical zygapophysial (facet) joints. Dr. Bogduk states:
“Collectively, these various biomechanics studies, in normal volunteers and in cadavers, predict or produce the same spectrum of lesions as that identified in postmortem studies. In particular, they indicate that the zygapophysial joints can be injured.”
“The zygapophysial joints are the single, most common source of pain in patients with chronic neck pain after whiplash.”
There is an extensive amount of evidence indicating that post-whiplash pain syndrome is attributed to injury to the cervical facet joints; no other explanation for whiplash pain has more evidence.
•••••••••
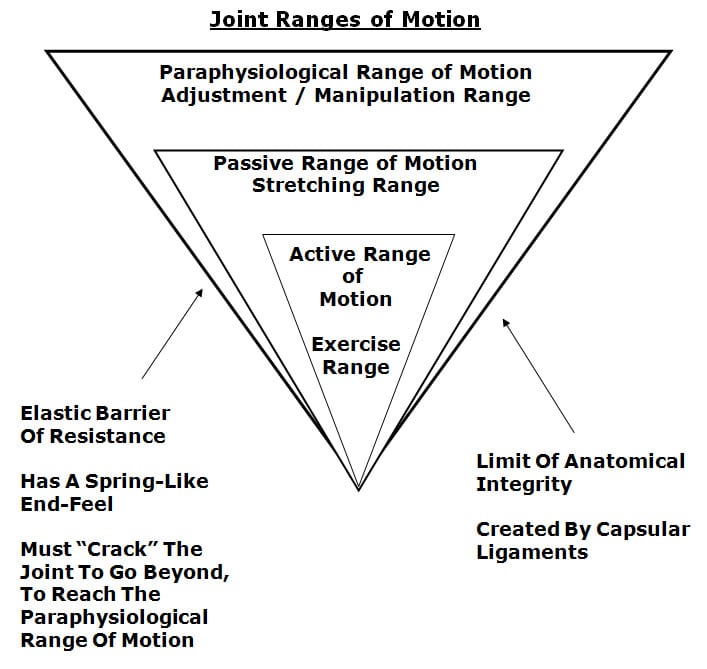
Mechanically, spinal manipulation primarily affects the spinal facet joints. This is well accepted and not controversial. In 1985, Canadian Orthopedic Surgeon, WH Kirkaldy-Willis, MD, stated (11):
“Spinal manipulation is essentially an assisted passive motion applied to the spinal apophyseal and sacroiliac joints.”
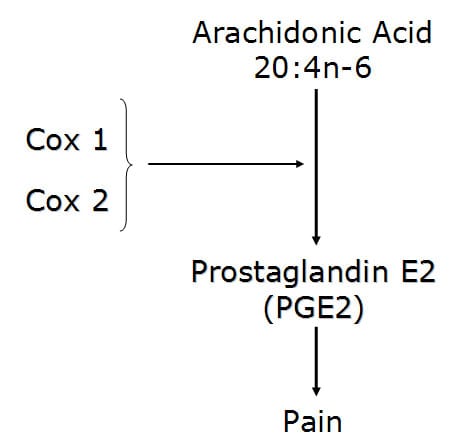
Biological Plausibility
- The primary injury from whiplash biomechanics is to the facet joints.
- The primary source of both acute and chronic whiplash injury pain is the facet joints.
- Spinal adjusting (specific joint manipulation) primarily affects the facet joints.
- It would appear to be biologically plausible that spinal adjusting could improve the pain status and recovery time of individuals injured in a whiplash type mechanism.
- Studies assessing such biological plausibility should show positive clinical outcomes.
A few pertinent studies are presented below:
In 1996, clinicians from the University Department of Orthopaedic Surgery, Bristol, United Kingdom, published a study in the journal Injury, titled (12):
Chiropractic Treatment of Chronic ‘Whiplash’ Injuries
The authors note, “The whiplash syndrome is a cause of long-term symptoms for which conventional medicine has failed to discover an effective treatment.” They note that 43% of patients will suffer long-term symptoms following ‘whiplash’ injury, for which no conventional treatment has proven to be effective. Consequently, they performed a retrospective study to determine the effects of chiropractic spinal manipulation [a nonconventional treatment] in a group of 28 patients who were suffering with chronic ‘whiplash’ syndrome. The authors defined “spinal manipulation” as:
“Spinal manipulation is a high-velocity low-amplitude thrust to a specific vertebral segment aimed at increasing the range of movement in the individual facet joint, breaking down adhesions and stimulating production of synovial fluid.”
The severity of patient’s symptoms was assessed before and after treatment using the Gargan and Bannister (1990) classification protocol, as follows:
The Gargan and Bannister Whiplash Classification
| GROUP | SYMPTOMS |
| A | None |
| B | Nuisance |
| C | Intrusive |
| D | Disabling |
The 28 patients in this study had initially been treated with anti-inflammatories, soft collars and physiotherapy. These patients had all become chronic, and were referred for chiropractic at an average of 15.5 months (range was 3–44 months) after their initial injury. At the initial evaluation and prior to chiropractic treatment, 27/28 (96%) of the patients were classified as category C (intrusive) or D (disabling) symptoms.
Following the chiropractic treatment, 93% of the patients had improved: 16/28 (57%) improved by one symptom group, and 10/28 (36%) improved by two symptom groups. The authors concluded:
“The encouraging results from this retrospective study merit the instigation of a prospective randomized controlled trial to compare conventional with chiropractic treatment in chronic ‘whiplash’ injury.”
“The results of this retrospective study would suggest that benefits can occur in over 90% of patients undergoing chiropractic treatment for chronic whiplash injury.”
•••••••••
In 1999, the same group of clinicians from the University Department of Orthopaedic Surgery, Bristol, United Kingdom, published a study in the Journal of Orthopaedic Medicine, titled (13):
A Symptomatic Classification of Whiplash Injury and the Implications for Treatment
In this study, the author’s objective was to determine which patients with chronic whiplash would benefit from chiropractic treatment. The study was a retrospective review involving 93 consecutive whiplash-injured patients. Once again, the patients were assessed using the Gargan and Bannister classification protocol. The authors note:
“Conventional treatment of patients with whiplash symptoms is disappointing.”
“In chronic cases, no conventional treatment has proved successful.”
All patients underwent spinal manipulation, defined as a “high velocity, low amplitude thrust to a specific vertebral segment.” Patients underwent a mean of 19.3 treatments (range 1-53), over a period of 4.1 months.
The authors note that their results “confirm the efficacy of chiropractic, with 69 of our 93 patients (74%) improving following treatment.” Importantly, 94% of whiplash patients with neurological signs and/or symptoms in association with neck pain and a restricted range of neck movement, including tingling, numbness, pins and needles in a dermatomal distribution in the arm or hand as well as both hypo- and hyperaesthesia, responded positively to chiropractic spinal manipulation. The authors concluded:
“The results from this study provide further evidence that chiropractic is an effective treatment for chronic whiplash symptoms.”
“Chiropractic is the only proven effective treatment in chronic [whiplash] cases.”
•••••••••
In 2004, a group of physiotherapists, physicians, and professors from the Rey Juan Carlos University, Spain, published a study in the Journal of Whiplash & Related Disorders, titled (14):
Manipulative Treatment vs. Conventional Physiotherapy Treatment in Whiplash Injury: A Randomized Controlled Trial
The authors note that the clinical syndrome of whiplash includes neck pain, restriction of neck motion, dizziness, headaches, tinnitus and blurred vision. Spinal joint dysfunction and myofascial pain syndrome are thought to be one of the greatest causes of musculoskeletal disorders and symptoms in patients diagnosed with whiplash injury.
The goal of joint manipulation is to restore maximal, pain-free movement of the musculoskeletal system. “Only joints that are found to be hypomobile should be considered as candidates for high velocity low amplitude [manipulative] techniques.”
The objective of this clinical trial was to compare the results obtained from a manipulative protocol with the results obtained from a conventional physiotherapy treatment in patients suffering from whiplash injury. This is the first controlled experimental trial documenting the effects of the manipulative protocol used in this study. It was a randomized controlled trial using 380 acute whiplash injury (less than 3 months duration) subjects. All subjects were Quebec Task Force classified as grades II and III.
- Quebec GRADE II = neck complaint and musculoskeletal signs
- Quebec GRADE III = neck complaint, musculoskeletal signs, and neurologic signs
The injured subjects were randomly divided into 2 groups:
Group A (experimental, manipulation group)
This group was treated with high velocity-low amplitude spinal manipulation and soft tissue manipulation. The manipulation was delivered to the upper cervical spine, the cervical-thoracic junction, thoracic spine, thoracolumbar junction and pelvic girdle. Importantly, although the patients were suffering from neck pain and related symptoms, the manipulation was applies “full spine.” The treatment was weekly.
Group B (control, physical therapy group)
This group was treated with a conventional physiotherapy including active exercises, electrotherapy, ultrasound therapy and diathermy. The treatment was daily.
The outcome measures were the visual analogue scale (VAS), the cervical range of motion (CROM) in flexion and rotation, and number of sessions needed to complete the treatment.
Analysis of the change in visual analogue scale for pain showed:
- The manipulation group obtained an average decrease of 40% in head and neck pain in 4 visits. (maximum improvement was 9 ± 1.5 visits)
- The physical therapy group, obtained a decrease of 19% after 10 visits. (maximum improvement was 23 ± 3.2 visits)
Analysis of the change in cervical range of motion showed:
- An improvement of 20° in cervical rotation, and 17.5° in cervical flexion after 4 sessions of spinal manipulation.
- An improvement of 2.5° in cervical rotation, and 6° in cervical flexion after 10 sessions of physical therapy.
| Spinal Manipulation | Physiotherapy | |
| Number of Visits | 4 | 10 |
| Decrease in Neck/Head Pain |
40% | 19% |
| Increase ROM Rotation |
20° | 2.5° |
| Increase ROM Flexion |
17.5° | 6° |
| Number of Visits to Maximum Improvement | 9 ± 1.5 | 23 ± 3.2 |
The authors note:
“Patients who had received manipulative treatment needed fewer sessions to complete the treatment than patients who had received physiotherapy treatment.”
“Patients of manipulative group needed an average of 9 sessions to complete the treatment, whereas physiotherapy group needed an average of 23 sessions.”
“Results showed that the manipulative group had more benefits than the physiotherapy group in the VAS and CROM.”
“Our clinical experience with these [whiplash-injured] patients has demonstrated that manipulative treatment gives better results than conventional physiotherapy treatment.”
Interestingly and importantly, these authors propose that it is “necessary to manipulate a number of spinal levels” to obtain the best outcomes for the whiplash-injured patient. Thoracic spine joint dysfunction may cause secondary adaptive or maladaptive changes in cervical and sacroiliac joints. Such adaptative changes in the cervical spine may contribute to the resulting headaches and neck pain in these patients. They note that whiplash injury symptoms (head, neck and upper thoracic pain) decrease in response to a thoracic spinal manipulation.
Also, in a rear-end impact, as the struck vehicle is accelerated forward, the seatback contacts the lumbo-pelvic region, causing compression and extension. “This compression of the lumbo-pelvic region produces a hypomobility in the pelvic girdle that is necessary to manipulate.”
This study emphasizes the need to use spinal manipulation to multiple spinal regions, including the pelvis, to obtain the best outcomes in the whiplash-injured patient. This is consistent with the perspective of rheumatologist John Bland, MD, from the University of Vermont College of Medicine. Note the following quote from his his book Disorders of the Cervical Spine (15):
“We tend to divide the examination of the spine into regions: cervical, thoracic, and lumbar spine clinical studies. This is a mistake. The three units are closely interrelated structurally and functionally – a whole person with a whole spine. The cervical spine may be symptomatic because of a thoracic or lumbar spine abnormality, and vice versa! Sometimes treating a lumbar spine will relieve a cervical spine syndrome, or proper management of cervical spine will relieve low backache.”
This is the first study showing the effectiveness of spinal manipulation in the management of acute whiplash injuries (the prior studies pertained to chronic whiplash injuries). In this study, spinal manipulation was significantly more effective both subjectively and objectively in treating Quebec Task Force whiplash injuries Grades II and III than conventional physiotherapy. These authors concluded:
“This clinical trial has demonstrated that head and neck pain decrease with fewer treatment sessions in response to a manipulative treatment protocol as compared to a physiotherapy treatment protocol among patients diagnosed with acute whiplash injury.”
Manipulation is “effective in the management of whiplash injury.”
“Manipulative treatment is more effective in the management of whiplash injury than conventional physiotherapy treatment.”
•••••••••
Recently (September 2015), researchers and clinicians from the Orthopedic University Hospital Balgrist, University of Zurich, Switzerland, published a study in the Journal of Manipulative and Physiological Therapeutics, titled (16):
Prognostic Factors for Recurrences in Neck Pain Patients
Up to 1 Year After Chiropractic Care
This is a prospective cohort study assessing 545 neck pain patients. After a course of chiropractic spinal manipulation, they were followed up for one year regarding recurrence of their neck pain. Nine independent prognostic variables were assessed:
- Age
- Use of pain medication
- Sex
- Work status
- Duration of complaint
- Previous episodes of neck pain
- Trauma onset
- Numeric Rating Scale (NRS) was used to quantify their pain
- Bournemouth Questionnaire was used for neck pain
These authors note that most people will see a health care provider at least once in their lifetime due to neck pain. In patient populations that do not include chiropractic care, those who have experienced an episode of neck pain are likely to have another episode within the next 1 to 5 years. Overall, for these individuals, the prognosis for a complete recovery from their neck pain is “quite poor.” Those who do not recover from their neck pain within the 3 months after treatment begins tend to suffer from residual neck pain and disability.
There are known prognostic factors for the onset of neck pain. They include:
- Computer work
- Heavy physical work
- Longer duration of complaint
- Older age
- Female sex
- Previous neck injury
The results of this study are impressive:
- Fifty-four (54) participants (11%) were identified as “recurrent.”
- Four hundred ninety one (491) participants (89%) were not recurrent.
The authors state:
“89% of neck pain patients had recovered from their neck pain episode up to 1 year after receiving chiropractic care.”
This study also found that older age and a previous episode of neck pain were useful predictors of neck pain recurrence within 1 year. This is because an increase in age was associated with recurrence. Patients older than 45 years are twice as likely to experience a neck pain recurrence within 1 year after the start of chiropractic treatment. They state:
“Having had a previous episode as well as increasing age are increased risk factors for predicting a subsequent new episode of neck pain within a year.”
These authors concluded:
“The results of this study suggest that recurrence of neck pain within 1 year after chiropractic intervention is low.”
This study indicates that chiropractic is both effective in the treatment of neck pain and that its benefits are stable and long lasting.
•••••••••
SUMMARY
Both acute and chronic neck pain is primarily attributed to the facet joints. This is especially true of those injured in a whiplash-mechanism accident. Chiropractic spinal adjusting (specific joint manipulation) affects many tissues, but primarily the facet joints. Evidence continues to support that spinal manipulation is both effective and safe for patients suffering with neck pain, including patients with neck pain initiated by a whiplash injury. The evidence supports spinal manipulation for both acute and chronic neck pain/. The evidence also shows that spinal manipulation is not only effective, but the benefits are also long-lasting with only a small incidence of recurrence.
REFERENCES
- Grauer JN, Panjabi MM, Cholewicki J, Nibu K, Dvorak J; Whiplash produces an S-shaped curvature of the neck with hyperextension at lower levels; Spine; November 1, 1997; Vol. 22; No. 21; pp. 2489-94.
- Kaneoka K, Ono K, Inami S, Hayashi K; Motion analysis of cervical vertebrae during whiplash loading; Spine; April 15, 1999; Vol. 24; No. 8; pp. 763-9.
- Schofferman J, Bogduk N, Slosar P; Chronic whiplash and whiplash-associated disorders: An evidence-based approach; Journal of the American Academy of Orthopedic Surgeons; October 2007; Vol. 15; No. 10; pp. 596-606.
- Uhrenholt L, Grunnet-Nilsson N; Hartvigsen J; Spine; Cervical spine lesions after road traffic accidents: a systematic review; September 1, 2002; Vol. 27; No. 17; pp. 1934-1941.
- Pearson AM, Ivancic PC, Ito S, Panjabi MM; Facet joint kinematics and injury mechanisms during simulated whiplash; Spine; February 15, 2004; Vol. 29; No. 4; pp. 390-397.
- Bogduk N, Aprill C; On the nature of neck pain, discography and cervical zygapophysial joint blocks; Pain; August 1993; Vol. 54; No. 2; pp. 213-217.
- Barnsley L, Lord SM, Wallis BJ; Bogduk N; The prevalence of chronic cervical zygapophysial joint pain after whiplash; Spine; January 1, 1995; Vol. 20; No. 1; pp. 20-25.
- Lord SM, Barnsley L, Wallis BJ; Bogduk N; Chronic cervical zygapophysial joint pain after whiplash. A placebo-controlled prevalence study; Spine; August 1, 1996; Vol. 21; No. 15; pp. 1737-1744.
- Bogduk N; On Cervical Zygapophysial Joint Pain After Whiplash; Spine December 1, 2011; Vol. 36; No. 25S; pp. S194–S199.
- Quinn KP, Winkelstein BA; Detection of Altered Collagen Fiber Alignment in the Cervical Facet Capsule After Whiplash-Like Joint Retraction; Annals of Biomedical Engineering; August 2011; Vol. 39; No. 8; pp. 2163–2173.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low back Pain; Canadian Family Physician; March 1985; Vol. 31; pp. 535-540.
- Woodward MN, Cook JCH, Gargan MF, and Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; Vol. 27; No. 9; November 1996; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999; pp. 22-25.
- Fernández-de-las-Peñas C, Fernández-Carnero J, Palomeque del Cerro L, Miangolarra-Page JC; Manipulative Treatment vs. Conventional Physiotherapy Treatment in Whiplash Injury: A Randomized Controlled Trial; Journal of Whiplash & Related Disorders; 2004; Vol. 3; No. 2.
- Bland J; Disorders of the Cervical Spine; WB Saunders Company; 1987; p. 84. [Professor of Medicine, University of Vermont College of Medicine].
- Langenfeld A, Humphreys K, Swanenburg J, Cynthia K. Peterson CK; Prognostic Factors for Recurrences in Neck Pain Patients Up to 1 Year After Chiropractic Care; Journal of Manipulative and Physiological Therapeutics; September 2015; Vol. 38; No. 7; pp. 458-464.